Suʻesuʻega Faʻapitoa-Faʻamālōlōina mo Aafiaga Faʻafuaseʻi Faʻafuaseʻi i El Paso, TX
O le aʻafia i se faʻalavelave faʻafuaseʻi o se tulaga e le manaʻomia lea e mafai ona mafua ai le tele o faʻalavelave faʻaleagaina poʻo manuaga faʻapea foi i le atinaʻeina o le tele o tulaga faʻaleagaina. O manuʻa faʻafuaseʻi faʻafuaseʻi, e pei o le afaina, e mafai ona faʻaalia i faʻamaʻi tiga, e aofia ai le tiga o le ua faʻavaivai, ae peitai, o suesuega o suʻesuʻega talu ai nei ua iloa ai o le faʻalavelave faʻalagona e afua mai i le osofaʻiga a le tagata lava ia e ono mafai ona faʻaalia i le tino. O le atuatuvale, atuatuvalega, atuatuvale ma le le mautonu o le maʻi, poo le PTSD, o faafitauli masani o le mafaufau e mafai ona tulai mai ona o se faalavelave tau taavale.
Na suʻesuʻeina foʻi e le au suʻesuʻe o suʻesuʻega suʻesuʻega e mafai ona avea togafitiga o le mafaufau ma le mafaufau e avea ma togafitiga lelei mo lagona mafatiaga ma mafaufauga e mafai ona tupu ona o se faʻalavelave lavea i le moli. E le gata i lea, o manuʻa faʻafuaseʻi i le oso faʻafuaseʻi atonu e mafua ai le atuatuvale, atuatuvale, atuatuvale ma e oʻo lava i le PTSD pe a le toe togafitia mo se taimi umi. O le faʻamoemoe o le tusiga o loʻo i lalo o le faʻaalia lea o aʻafiaga o togafitiga faʻamalosi-amio, faatasi ai ma isi togafitiga togafitiga e pei o togafitiga faʻasolosolo ma togafitiga faʻapitoa. mo faʻalavelave faʻafuaseʻi faʻafuaseʻi, e pei o le sasa.
Tinoina o le tino, Gaioiga Faʻasino ma le Malamalama-Gaioiga Gaoioiga e Fai ma Togafitiga mo Tupulaga Talavou Matutua O tagata mamaʻi ma le Faʻanoanoa o Paʻu: Faʻailogaina o le Faʻatonuina o le Faʻatonuina o le Faʻatonu
lē faʻatino
tua
O le tele o tagata gasegase e mafatia i le tiga o le ua masani i le maeʻa ai o se manua. O se tuufaatasiga o togafitiga o le mafaufau, amio ma togafitiga o le physiotherapy ua faailoa mai ina ia aoga i le puleaina o tagata gasegase e le masani ona afaina ai le toto. O le faʻamoemoe o le tuʻuina atu lea o le mamanu o se faamasinoga faʻatonuina (RCT) e fuafua i le iloiloga o le aoga o se faʻavae faʻapitoa i le tino ma le mafaufauina o amioga i luga o le faʻatinoina o galuega faʻapitoa i le tagata lava ia, e faaopoopo i le galuega o le ua, tiga, le atoatoa ma tulaga lelei o le soifuaga i tagata mamaʻi ma le tiga masani o le ua i le maea ai o le manua o le gau i le faʻatusatusa atu i se kulupu o loʻo faʻatusatusa i fuataga ma 4 ma 12 masina pe a maeʻa.
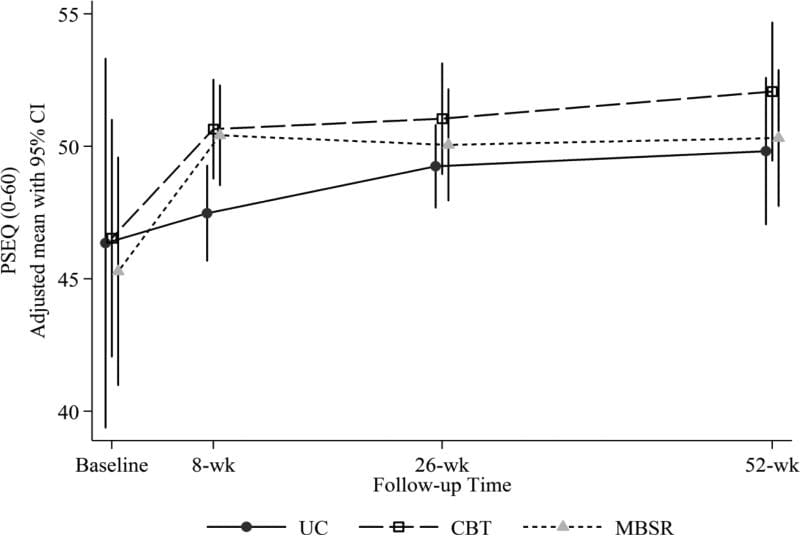
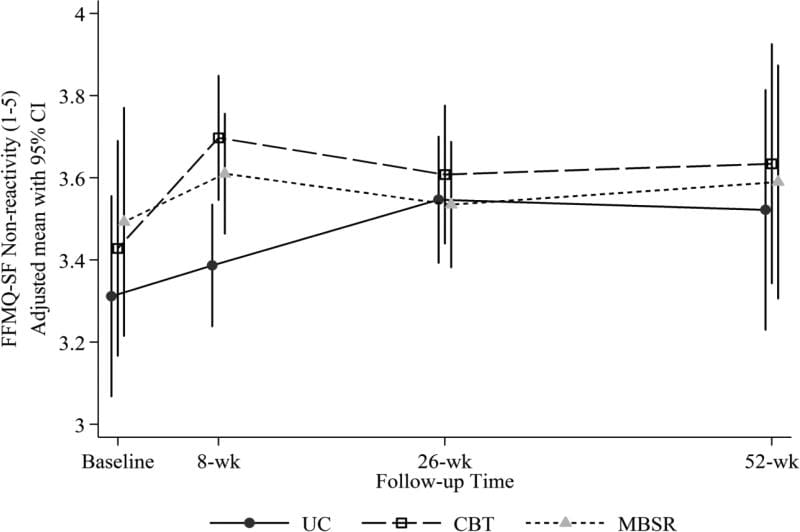
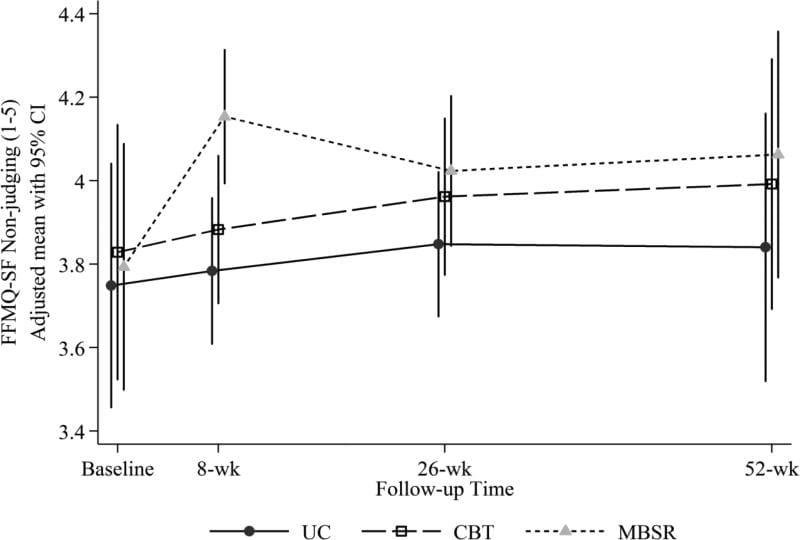
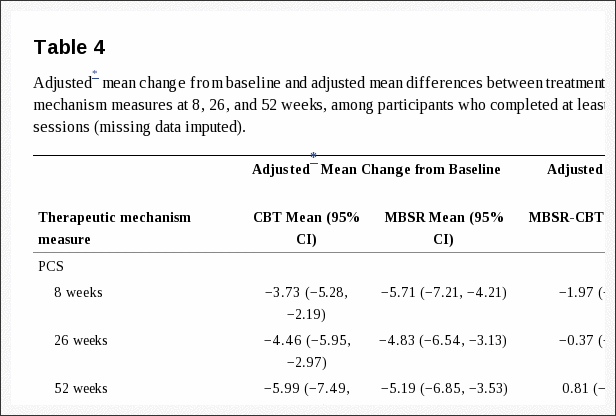
Metotia / Fuafuaga
O le mamanu o se suʻesuʻega lua-tutotonu, RCT-suʻesuʻe ma se mamanu faʻavae tutusa. E aofia ai faʻamaʻi pipisi ma le tiga o le ua faʻavaivaia mo le sili atu nai lo le 6 masina, na maua mai i falemaʻi o le physiotherapy ma le falemaʻi i fafo i Tenemaka. O tagata maʻi o le a faʻaaogaina i se vaega o le puleaina o le tiga (pule) poʻo se tuʻufaʻatasia o mea tiga ma faʻasalalauga. O le vaega faʻaleaʻoaʻoga o le a maua ni vasega faʻaleaʻoaʻoga se fa i le puleaina o tiga, ae o le vaega faʻapitoa o le a maua ia lava aoaoga faʻaleaʻoaʻoga i luga o pulega o tiga ma le 8 fonotaga mo toleniga mo masina 4, e aofia ai le faʻataʻitaʻiga i ni tino faapitoa o le tino ma se polokalame faʻaleaʻoaʻoga tau vaʻaia. O maʻi ma fomaʻi ua iloa lelei le tufatufa ma le togafitiga, aʻo faʻatauasolo faatonu ma tagata suʻeina faʻamaumauga. O fua muamua o fuataga o le a avea ma Fomaʻi Suʻesuʻega o Suʻesuʻega o Togafitiga Fomaʻi 36 (SF36), Aotelega Faʻatino Autu (PCS). Maualuga taunuʻuga o le a maua i le Global Enquiry Implementation (-5 to + 5), Index Neck Disability Index (0-50), Scale Specific Functioning Scale (0-10), scale rating scale for pain depression (0-10), SF-36 Mental Aotelega Faʻatonu (MCS), TAMPA fua o Kinesiophobia (17-68), Faʻafitauli o Fua Faʻatulagaga (0-45), EuroQol (0-1), Testing Flexible Craniocervical (22 mmHg - 30 mmHg), test test position and cervical ituaiga o feoaiga. O sikola SF36 o loʻo faʻaaoga e faʻaogaina ai auala faʻavae masani ma PCS ma MCS o loʻo i ai le fuainumera o le 50 faʻatasi ai ma se faʻasologa masani o le 10.
Talanoaga
O faʻamatalaga o lenei suʻesuʻega e talanoaina, faʻaopopo i malosiaga ma vaivaiga.
Faʻamaumauga o le suʻega
O loʻo suʻesuʻeina le suʻesuʻega www.ClinicalTrials.gov e faailoa NCT01431261.
tua
Ua fuafua e le Komiti o le Health Board Board a le Danish e faapea o mataupu 5-6,000 i tausaga taʻitasi i Tenimaka e aafia i se faalavelave faʻafuaseʻi e faʻafefe ai le tiga ole ua. E uiga i le 43% oi latou o le ai ai pea le faaletonu faaletino ma faailoga 6 masina pe a mavae le faalavelave [1]. Mo sosaiete Suetena, e aofia ai kamupanī inisiua Suetena, o le avega o le tamaoaiga e tusa ma le 320 miliona Euros [2], ma o lenei avega e foliga tutusa ma lena o Tenimaka. O le tele o suʻesuʻega o loʻo fautua mai ai o tagata na maua i le Whiplash-Associated Disorders (WAD) latou te lipotia le faʻamalologa o le kuli i le tausaga e tasi talu ona faʻaleagaina [3]. Ole faafitauli ogaoga i tagata mamaʻi ma le tiga o le tiga o le tiga ole tino ole gasegase ma le le talafeagai ole gaioiga o le ua, faaitiitia le malosi o le ua ma le mausali, faaletonu cervicocephalic lagona faaanamua, e faaopoopo atu ile tigaina o le lotoifale ma le lautele [4,5]. O le maʻi o le tino e faʻaalia i le faʻaititia o le gaioiga o maso malolosi o le ua.
E ese mai i le tiga o le ua masani, o maʻi ma le WAD e mafai ona mafatia mai le le atoatoa o le tino ona o se taunuuga o le tiga faaumiumi [6,7]. O lenei mea e aʻafia ai le soifua maloloina faaletino ma le soifua maloloina lautele ma e mafai ona iu i se tulaga leaga o le olaga. I le faʻaopoopoga, e mafai e tagata atiaʻe WAD ona maua le tiga faʻapitoa e mulimuli mai i le faʻalogoina o le tino o le tino [8,9], i le faʻaitiitia o le faitotoʻa mo mea eseese faʻapitoa (mamafa, malulu, mafanafana, vibration ma pulupulu eletise) [10]. O lenei mea e mafai ona mafua mai i le le mautonu o le faʻasaina o le totonugalemu o le tino [11] - o se toe faʻafouina o le tino [12]. E ese mai i le tulaga tutotonu tutotonu, o le vaega o loʻo i ai le OFA e ono itiiti lava le faʻaogaina o auala faʻataʻitaʻiga ma galuega felagolagomaʻi, pe a faʻatusatusa atu i tagata mamaʻi o loʻo faʻavaivaia le tiga o le tino i le lautele [13-15].
O suʻesuʻega ua faʻaalia ai o toleniga faʻapitoa, e aofia ai faʻamalositino patino e tulimataʻia ai maso o loʻo i lalo o le tui o le tino, e lelei le faʻaitiitia o le tiga o le tino [16-18] mo tagata mamaʻi ma le tiga o le ua masani, e ui lava e iai se fesuiaiga i le tali i le aʻoga ae le tagata maʻi uma e faʻaalia se suiga tele. O le gaioiga faʻale-tino e gaosia ai le tino o se togafitiga togafitiga ma le taulaʻi i le faʻateleina o le tino faaletino, faʻaitiitia le fefe i le fegasoloʻiga ma le faʻaleleia o le mafaufau [19,20]. E le lava le faʻamaoniga mo le faʻaauau pea o le togafitia o togafitiga faʻale-tino ma le mafaufau, aemaise lava i le faʻavave o maʻi o le ua. O aʻoaʻoga faʻaleaʻoaʻoga, o le mea e taulai i ai le malamalama i faʻalavelave ogaoga o le tiga o le tino ma le atinaʻeina o le talafeagai o le tigaina ma / poʻo le faʻataʻitaʻiga o amio, ua faʻaalia ai le faʻaitiitia o le tiga lautele [6,21-26]. O se iloiloga na faailoa mai ai o gaioiga faatasi ai ma le tuufaatasiga o faamalositino, amio pulea ma le togafitiga e aofia ai faamaʻi tino, e aoga i le puleaina o tagata mamaʻi WAD ma le tiga o le tiga o le tiga [27], e pei foi ona fautuaina e taiala Dutch mo le WAD [28]. Ae ui i lea, o faaiuga e faʻatatau i taʻiala e faʻavae tele lava i luga o suʻesuʻega na faia i luga o tagata gasegase i ai le tele o le WAD [29]. O se faaiuga sili atu ona tuusaʻo na maua mai i tagata mamai o le WAD o loʻo i ai pea le tiga i le Bone ma le Joint Decade 2000-2010 Task Force, ma fai mai, 'talu ai ona o feteʻenaʻiga molimau ma nai suʻesuʻega maualuga, e leai ni faaiuga mausali e mafai ona maua e uiga i le sili ona lelei -o faʻasalaga faʻaleagaina mo tagata gasegase e masani ona faia i le aso "[29,30]. O le manatu o togafitiga tuʻufaʻatasia mo tagata mamaʻi WAD e maua ai le tiga tumau na faʻaaogaina i se faamasinoga muamua na faʻatautaiaina [31]. O taunuuga na faailoa mai ai o le tuufaatasiga o faiga faamalositino e aunoa ma se faapitoa ma fautuaga e aofia ai aʻoaʻoga o tiga ma le faamautinoaga ma le faamalosiauga e toe faaauau ai le malamalama, na maua ai ni taunuuga e sili atu nai lo fautuaga mo na o tagata mamaʻi i le WAD 3 masina talu le faalavelave. O gasegase na faʻaalia le faʻaleleia o le ogaoga o le vevela, tiga o le faʻalavelave ma galuega i gaioiga i aso taʻitasi i le vaega o loʻo maua le faʻamalositino ma fautuaga, pe a faatusatusa i fautuaga. Ae ui i lea, o le alualu i luma na laiti ma na o le manino i le taimi pupuu.
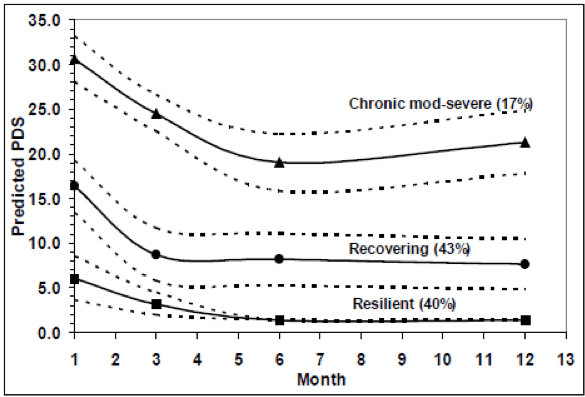
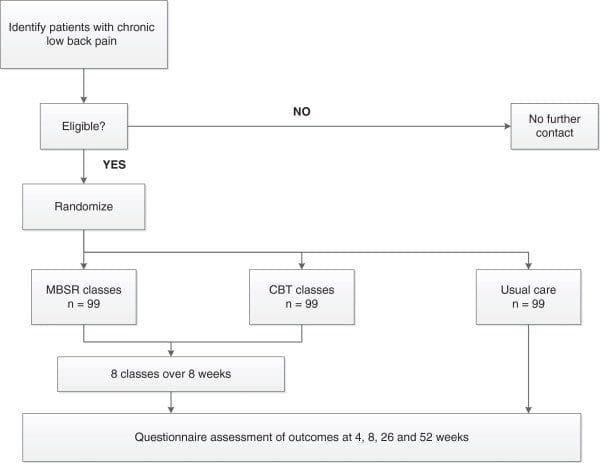
O lenei poloketi na fausia i luga o le faʻamoemoe o le toe faʻaleleia o le WAD tagata mamaʻi ma le tiga o le ua e tatau ona faʻatatau i le faʻaʻautagata, toleniga o faʻamalositino gaioiga ma le malamalama ma le puleaina o tiga tumau i se tuʻufaʻatasia togafitiga auala. O faʻalavelave taʻitasi e faʻavae i luga o suʻesuʻega muamua na faʻaalia ai le aoga [6,18,20,32]. Lenei suʻesuʻega o le muamua e aofia ai foʻi le umi o aʻafiaga o le tuʻufaʻatasia o faʻataʻitaʻiga i tagata mamaʻi ma le tumau o le ua i tua pe a uma le sasa faʻafuaseʻi. E pei ona atagia i le Ata? Ata1,1, o le faʻataʻitaʻiga faʻavae i lenei suʻesuʻega e faʻavae i luga o le talitonuga o le toleniga (e aofia uma ai taʻiala taʻitasi faʻataʻitaʻiina o le ua ma aʻoaʻoina aerobic aʻoaʻoga) ma aʻoaʻoga i le puleaina o tiga (faʻavae i luga o le mafaufau faʻatino amioga amio) o sili atu mo le faʻateleina o tagata lelei 'tino lelei o le olaga, faʻatusatusa i aʻoaʻoga i tiga puleaina naʻo latou. Faateleina le tulaga lelei o le olaga aofia ai le faʻateleina o le lautele faʻagaioiga tino ma le tulaga o faʻamalositino, faʻaititia le fefe i gaioiga, faʻaitiitia o faʻailoga o le popolevale post-traumatic, faʻaititia le ua tiga ma faʻateleina ua galue. O le aʻafiaga e faʻamoemoe e maua vave i le maeʻa ai o togafitiga (ie 4 masina; puʻupuʻu aoga) faʻapea foʻi ma le tuanaʻi tasi le tausaga (long-term effects).
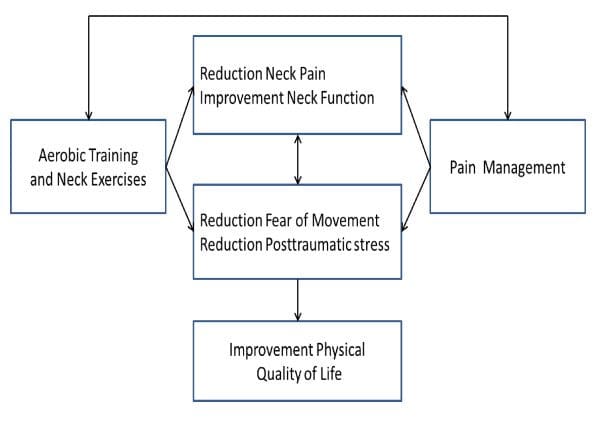
Ata 1: Vaʻaia o le aʻafiaga o aʻafiaga mo tagata gasegase i le faʻavaʻa o le ua i le maea ai o se faʻalavelave lavelave.
I le faʻaaogaina o se faʻataʻitaʻiga faʻapitoa (trial), o le faʻamoemoe o lenei suʻesuʻega o le iloiloga lea o le aoga o: aʻoaʻoga faʻapitoa i le tino, e aofia ai faʻamalosi faapitoa o le tino ma aʻoaʻoga faʻamalosi lautele, faʻatasi ai ma aʻoaʻoga i le puleaina o tiga (faʻavae i luga o se amioga faʻataʻitaʻi) aʻoga i le puleaina o tiga (faʻavaeina i luga o se amioga faʻataʻitaʻiga), fuaina o le tino faaletino o le olaga ', galuega faaletino, tiga o le ua ma le ua, le fefe i le feʻaveaʻiga, faʻaʻailoga post-traumatic ma le maualuga o le mafaufau o le olaga, i tagata mamaʻi tiga tiga pe a uma le manua o le whiplash.
Metotia / Fuafuaga
Faʻailoga o le Faʻamasinoga
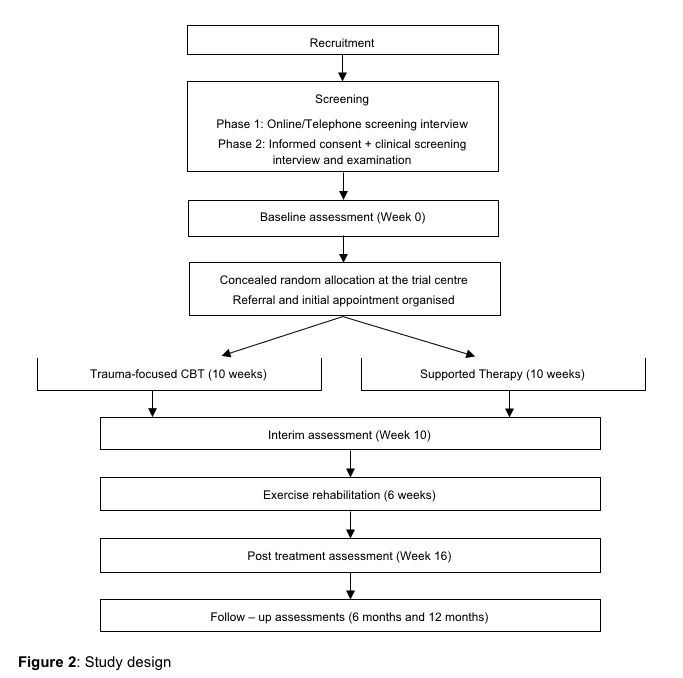
O le suʻesuʻega o loʻo faʻatautaia i Tenimaka o se RCT ma se tutusa kulupu mamanu. O le a avea ma lua-ogatotonu suʻesuʻega, faʻamaonia e tagata faigaluega suʻega. Tagata gasegase o le a faʻasolosolo i soʻo le Paʻu Pulega vaega (faʻatonutonu) poʻo le Paʻu Pulea ma Aʻoaʻoga kulupu (fesoasoani). E pei ona atagia i le Ata? Ata2,2, o le suʻesuʻega ua fuafuaina e aofia ai se tulaga lua faʻamaumauga suʻesuʻega 12 masina pe a maeʻa laina amata; o le muamua faʻaiuga iloiloga o le a faia i le taimi lava e maeʻa ai le polokalame fesoasoani 4 masina pe a maeʻa le faʻavaeina. O le suʻesuʻega faʻaaogaina se faʻasoaga faʻatupeina gaioiga, faʻamautinoaina o le kulupu e tuʻuina i ai le tagata maʻi e le o iloa ae le i ulufale le tagata onosaʻi i totonu o le suʻesuʻega. O faʻaiʻuga o suʻesuʻega ma faʻamatalaga suʻesuʻe o le a taofia le faʻatauasoina i le faʻasoaga i le faʻasoaga poʻo le faʻatonutonu kulupu.
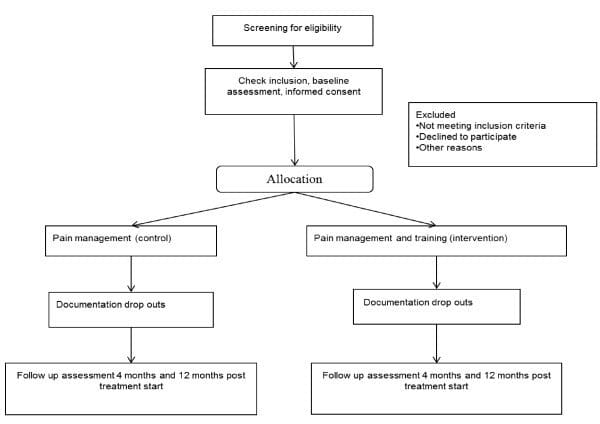
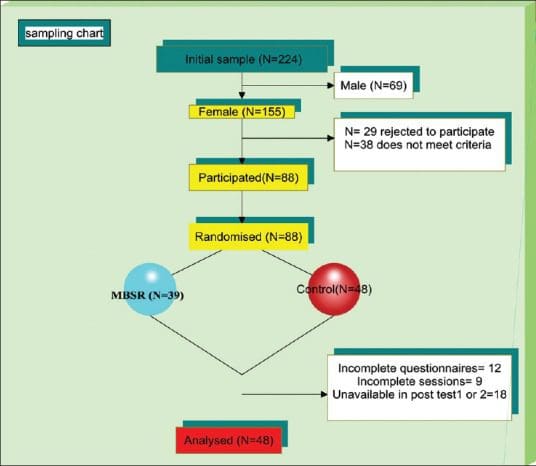
Ata 2: Taumalama o tagata gasegase i le suʻesuʻega.
tulaga
The participants will be recruited from physiotherapy clinics in Denmark and from The Spine Centre of Southern Denmark, Hospital Lilleb�lt via an announcement at the clinics and the Hospital. Using physiotherapy clinics spread across Denmark, the patients will receive the intervention locally. The physiotherapy clinics in Denmark receive patients via referral from their general practitioners. The Spine Centre, a unit specialising in treating patients with musculoskeletal dysfunctions and only treating out-patients, receives patients referred from general practitioners and/or chiropractors.
Suesue le faitau aofaʻi
Lua selau tagata matutua ma le laʻititi tausaga le 18 tausaga, mauaina togafitiga faʻasoifua maloloina pe ua uma ona faʻasino mo togafitiga o le tino o le a toe faʻafaigaluegaina. Mo tagata agavaʻa ia agavaʻa, e tatau ona i ai: tiga masani ua o le ua mo le le itiiti ifo i le 6 masina pe a maeʻa le sasaina o le manuʻa, faʻaititia le faʻamalositino gaioiga (Neck Disability Index score, NDI, o le itiiti ifo o le 10), tiga muamua i le ua eria, maeʻa soʻo se suʻesuʻega / faʻataʻitaʻiga o leitio, o le mafai faitau ma malamalama ia Tenimaka ma le agavaʻa e auai i le polokalame faʻamalositino. O tuʻutuʻuga faʻavae aofia ai: neuropathies / radiculopathies (faʻataʻitaʻi faʻapitoa e: lelei Spurling, faʻaʻautagata gaioiga ma plexus brachialis faʻataʻitaʻiga) [33], neurological deficits (tofotofoina e pei o masani falemaʻi faʻataʻitaʻiga e ala i le faʻagasologa o le suʻesuʻeina mo le iloa faʻapitoa), faʻatinoina i faʻataʻitaʻi faʻafomaʻi. togafitiga, o le i ai i se le maalofia agafesootai ma / pe o le faigaluega tulaga, maʻitaga, iloa gau, lotovaivai e tusa ai ma le Beck Depression Index (togi> 29) [18,34,35], po o isi lauiloa fomai soʻotaga tulaga e mafai ona matua taofia ai le auai i le polokalama faamalositino. O le a talosagaina le au auai e aua le sailia isi togafitiga o le tino poʻo le mafaufau togafitiga i le taimi o le vaitaimi aʻoga.
Faʻalavelave
pule
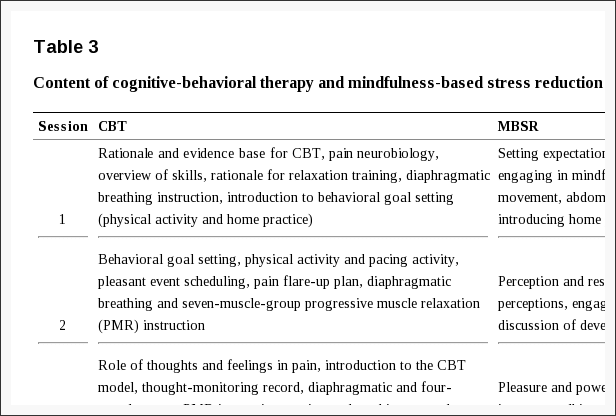
O le vaega o le Pain Management (control) vaega o le a maua aʻoaʻoga i metotia o le puleaina o tiga. O le ai ai ni 4 sessions o 11 / 2 itula, e aofia ai mataupu e uiga i faiga o tiga, taliaina o tiga, faʻaaogaina o taʻiala, ma le faʻatulagaina o sini, e faʻavae i luga o le faʻamalositinoina o le tiga ma le suʻesuʻeina o manatu [21,26,36].
Faʻalavelave
O le Pain Management plus Training (intervention) vaega o le a maua le aʻoga tutusa i le puleaina o tiga e pei oi latou o loʻo i totonu o le kulupu faʻatasi ma 8 togafitiga togafitiga (faʻaaogaina o faamaʻi ma aʻoaʻoga faʻaauau) faatasi ai ma le vaitaimi lava e tasi o le 4 masina. Afai e fuafuaina e le fomaʻi togafitiga togafitiga togafitiga faaopoopo, e mafai ona faʻalautele togafitiga faʻatasi ma 2 faʻasalalauga. Faʻalogoga i le tuli: O le togafitiga o faʻataʻitaʻiga faapitoa o le tino o le a alualu i luma e ala i vaega eseese, ia o loʻo faʻamatalaina e seti seti o le ua. I le taimi o togafitiga muamua, o suʻega e suʻeina mo le gaioio neuromuscular galuega e faʻamalamalama ai le tulaga patino lea e amata ai le aʻoga i le ua. O se polokalama faʻapitoa e faʻatinoina taʻitoʻatasi taʻitoʻatasi o le a faʻaaogaina e faʻamoemoe ai le ua faʻamalosi ma le maso. O le gafatia e faʻaosoina ai le manava loloto o le tino e faʻamalosi ai maso o le pito i luga o le potu e faʻateleina ai lo latou malosi, tutumau ma le mausali o le gaioiga faʻaleleia e ala i le faʻaaogaina o le gagana craniocervical i le faʻaaogaina o se faʻaliliuga faʻaalia o le biopressure [18,37]. O faamalositino mo le faapipiiina o mata, tulaga o le sooga, o le paleni ma le tutumau o le uaua, o le a aofia ai foi, ona ua faaalia ai le faaitiitia o le tiga ma faaleleia le puleaina o le tino i tagata mamaʻi ma le tiga o le tiga o le ua [17,38]. Aʻoaʻoga faʻamalositino: O le ogalaau tele ma vae o le a aʻoaʻoina i se polokalame faifaipea o le faʻaleleia o le tino. O tagata gasegase o le a faatagaina e filifili gaoioiga e pei o le savali, uila vilivae, savali savali, aau, ma le taʻavale. O le taʻiala mo le aʻoaʻoina o le taimi e faʻatulaga e ala i le faʻaaogaina o 3 taimi i se tulaga faʻalelei, e le faʻamalosia ai le tiga ma faʻamoemoe i se tulaga faʻamalosi ua fuafuaina (RPE) i le va o le 11 ma le 14 i luga o le fua o le Borg [39]. O le taimi muamua o aʻoaʻoga ua seti ai le 20% i lalo o le taimi masani o tofotofoga e tolu. O faʻasalalauga faʻapitoa e faia i aso faalua uma ma se mea e manaʻomia muamua e le o mamafa le tiga, ma o le RPE i le va o le 9 ma le 14. E faʻaaogaina se tusi faʻataʻitaʻiga. Afai e le o toe maua e se tagata maʻi se toe toso, ma lipoti mai se fua faatatau RPE ole 14 poʻo le itiiti, o le taimi faʻatinoina mo le vaitau o loʻo mulimuli mai (1 poʻo 2 vaiaso) e faʻateleina e minute 2-5, e oo atu i le maualuga o 30 minute. Afai o le RPE o le 15 poʻo le maualuga, o le a faʻaitiitia le taimi faʻatinoina i le fua o le RPE o le 11 i le 14 i le lua vaiaso [20,40]. I le faʻaaogaina o nei taʻiala, o le toleniga o le a faʻapipiʻiina e le tagata maʻi, faʻatasi ai ma le taulaʻi atu i taumafaiga faʻapitoa - faʻatasi ai ma le faʻamoemoe o le faʻateleina o le tulaga o le tino ma le malosi o le tino.
O le tausisia o tagata maʻi o le a faʻafoeina e ala i le lesitalaina o lo latou auai i le faʻafoega ma le faʻamaoniga o vaega. O tagata gasegase o le kulupu e pulea o le a iloiloina ua maeʻa le puleaina o tiga pe afai latou te auai i le 3 mai taimi o le 4. O le a faʻamaonia le maeʻaina o le vaega o loʻo aʻafia ai pe afai o le tagata maʻi na auai i le laʻititi o le 3 mai fonotaga a le 4 faʻamalositino ma se laʻititi o le 5 mai fonotaga a le 8. O toleniga a le tagata maʻi i le fale ma le faamalosi o le tino ma aʻoga faʻapitoa o le a faamauina e ia i totonu o se loka. O le tausisia o le 75% o le aʻoaʻoga fuafuaina i aiga o le a iloiloina e pei o le maeʻaina o le faʻaogaina.
Fomaʻi fomai
O le a faʻaaogaina i latou e le auai i le fomaʻi e ala i se faʻaliga i le Danish Physiotherapy Journal. O le faʻavaeina o maʻaʻoga e aofia ai le: avea ma se fomaʻi faʻapitoa, galue i se falemaʻi ma ia le itiiti ifo ma le lua tausaga o le galue galue o se fomaʻi, aʻo auai i se vasega i le faʻasalalauga faʻamatalaina ma pasia le suʻega e faatatau i ai.
Fua faʻatatau
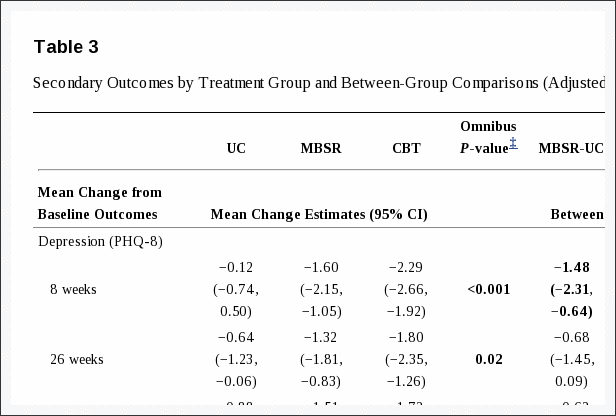
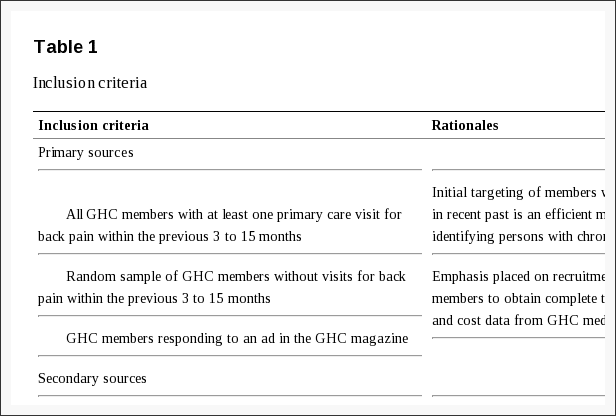
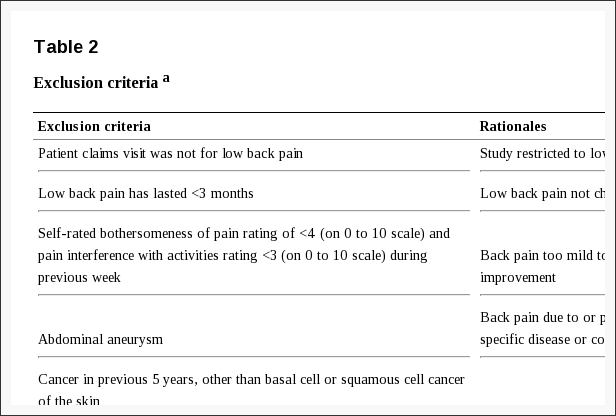
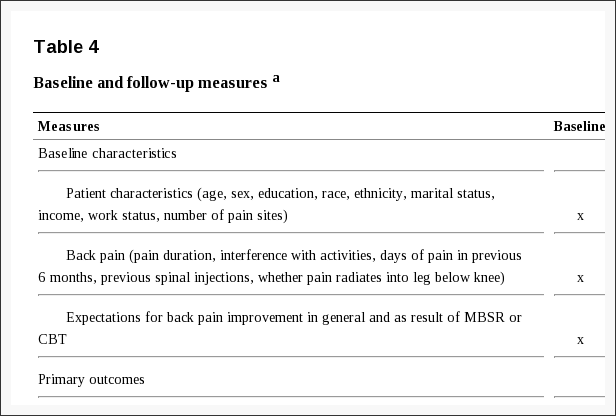
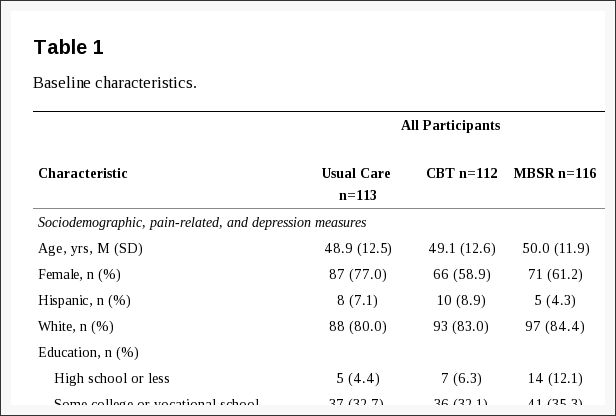
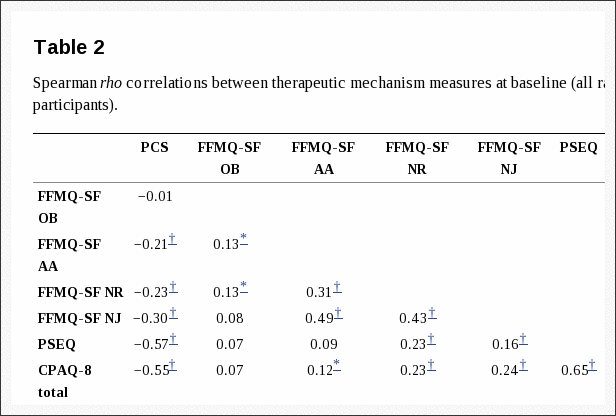
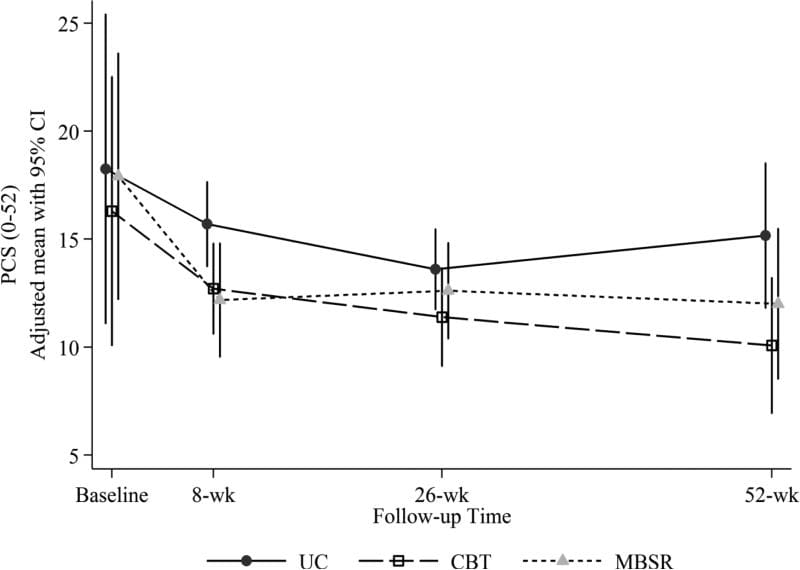
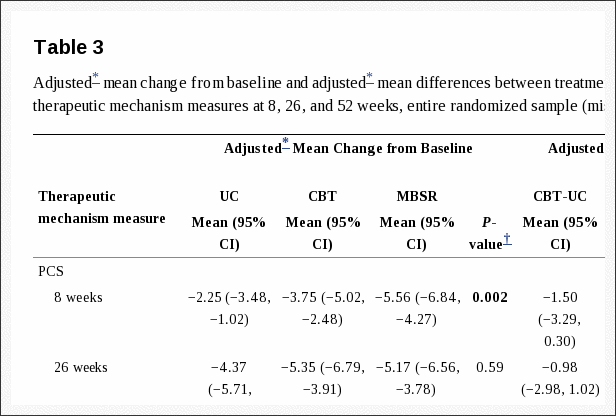
I le amataga o faʻamatalaga a le au auai i tausaga, itupa, maualuga ma le mamafa, ituaiga o faʻalavelave, vailaʻau, atinaʻe o faʻailoga i le lua masina talu ai (tulaga quo, faʻaleleia atili, faʻateleina), faʻamoemoeina o togafitiga, galuega ma aʻoaʻoga tulaga o le a lesitalaina. I le avea ai o se mautu muamua faʻataʻitaʻiga, Fomaʻi Aʻoga Suʻesuʻega Pepa Pepa 36 (SF36) - Tino Vaega o Aotelega (PCS) o le a faʻaaogaina [41,42]. O fua a le PCS e togiina e faʻaaogaina ai metotia faʻavae masani [43,44] ma le togi masani o le 50 ma le fesuiaʻiga masani o le 10. O le taunuʻuga autu e tusa ai ma le i ai o se aʻafiaga, o le a fuafuaina o se suiga mai le laina amata [45]. Tulaga lua taunuʻuga aofia faʻamaumauga luga uma faʻataʻitaʻi tofotofoga ma onosaʻi-lipotia taunuʻuga. Lisi? O loʻo faʻataʻitaʻi mai e le table11 suʻesuʻega o le falemaʻi mo le fuaina o le fesoʻotaʻiga i le neuromuscular puleaina o maso o le faʻaʻautagata, faʻaaogaina o le faʻaʻautagata ma le allodynia o masini. Laulau? O loʻo faʻailoa mai i le table22 taunuʻuga na maua mai i fesili na faʻaaoga e faʻataʻitaʻi ai le aʻafiaga o togafitiga, tiga o le ua ma le faʻagaioiga, tiga o le tiga, fefe i gaioiga, mafatiaga i tua atu o le faʻalavelave ma le lelei o le olaga ma ono mafai ai ona suia togafitiga.
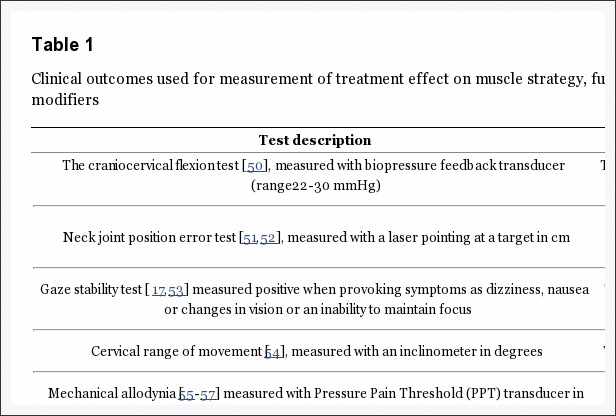
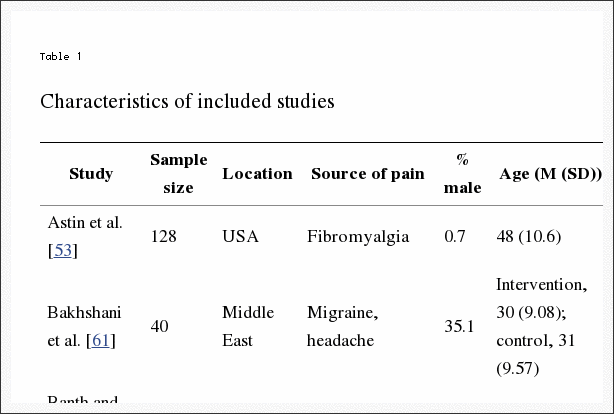
Laulau 1: Fomaʻi o taunuʻuga na faʻaaogaina mo le fuaina o togafitiga i togafitiga musika, galuega ma togafiti togafitiga.
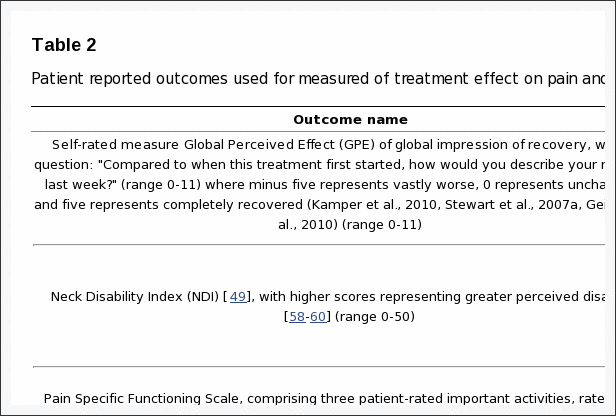
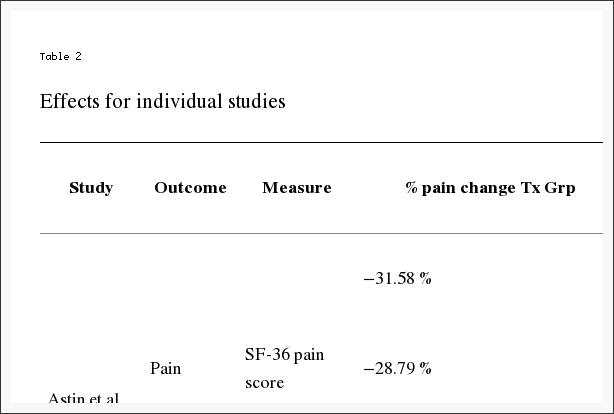
Laulau 2: Suʻega na lipotia lipoti na faʻaaogaina mo le fuaina o togafitiga i luga o tiga ma galuega.
O tagata maʻi o le a tofotofoina i le laina, 4 ma 12 masina i le maea ai o le laina, sei vagana ai GPE, lea o le a fuaina 4 ma 12 masina pe a uma le laina.
Malosiaga ma le Faataʻitaʻiga Fua Faatatau
The power and sample size calculation is based on the primary outcome, being SF36-PCS 4 months after baseline. For a two-sample pooled t-test of a normal mean difference with a two-sided significance level of 0.05, assuming a common SD of 10, a sample size of 86 per group is required to obtain a power of at least 90% to detect a group mean difference of 5 PCS points [45]; the actual power is 90.3%, and the fractional sample size that achieves a power of exactly 90% is 85.03 per group. In order to adjust for an estimated 15% withdrawal during the study period of 4 months, we will include 100 patients in each group. For sensitivity, three scenarios were applied: firstly, anticipating that all 2 � 100 patients complete the trial, we will have sufficient power (> 80%) to detect a group mean difference as low as 4 PCS points; secondly, we will be able to detect a statistically significant group mean difference of 5 PCS points with sufficient power (> 80%) even with a pooled SD of 12 PCS points. Thirdly and finally, if we aim for a group mean difference of 5 PCS points, with a pooled SD of 10, we will have sufficient power (> 80%) with only 64 patients in each group. However, for logistical reasons, new patients will no longer be included in the study 24 months after the first patient has been included.
Faʻamatalaga, Faʻasalaga ma Faʻatausologa Taualumaga
I le maeʻa ai o le iloiloga o le faavae, o le au auai e tuʻuina atu i se isi itu i le vaega o loʻo pulea poʻo le vaega o loʻo faʻaosoosoina. O le faasologa faasolosolo ua fausia e faaaoga ai le numera o fuainumera faamaumauina o le SAS (SAS 9.2 TS level 1 M0) ma ua faʻamaonia i le ogatotonu ma le 1: 1 faʻavae e faʻaaoga ai numera poloka poloka o 2, 4, ma 6. O le faasologa o le faasologa o le a natia mai le tagata suesue e lesitala ma iloiloina tagata auai i le faasologa o numera, opaque, faamaufaailoga ma faapipii ni teutusi. O le alumini alumini i totonu o le teutusi o le a faʻaaogaina e tuʻu ai le teutusi e le mafai ona faʻamalosia i le malamalama tele. A maeʻa ona faʻaalia mea o loʻo i totonu o le teutusi, e iloa uma e tagata gasegase ma fomaʻi le faʻavaeina ma le togafitiga talafeagai. O le au suʻesuʻega ma le aufaʻamaumauga o faʻamatalaga e ui i lea, o loʻo taofia taua. A o leʻi faia suʻesuʻega, o le a fesiligia e le suʻega suʻesuʻe le gasegase ia aua le taʻua le togafitiga na tuʻuina atu ia i latou.
Fuainumera Faamaumauga
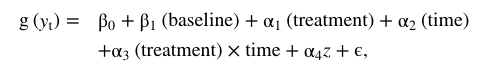
All the primary data analyses will be carried out according to a pre-established analysis plan; all analyses will be done applying SAS software (v. 9.2 Service Pack 4; SAS Institute Inc., Cary, NC, USA). All descriptive statistics and tests are reported in accordance with the recommendations of the ‘Enhancing the QUAlity and Transparency Of health Research’ (EQUATOR) network; i.e., various forms of the CONSORT statement [46]. Data will be analysed using a two-factor Analysis of Covariance (ANCOVA), with a factor for Group and a factor for Gender, using the baseline value as covariate to reduce the random variation, and increase the statistical power. Unless stated otherwise, results will be expressed as the difference between the group means with 95% confidence intervals (CIs) and associated p-values, based on a General Linear Model (GLM) procedure. All the analyses will be performed using the Statistical Package for Social Sciences (version 19.0.0, IBM, USA) as well as the SAS system (v. 9.2; SAS Institute Inc., Cary, NC, USA). A two-way analysis of variance (ANOVA) with repeated measures (Mixed model) will be performed to test the difference over time between the intervention and the control groups; interaction: Group � Time. An alpha-level of 0.05 will be considered as being statistically significant (p < 0.05, two- sided). The data analysts will be blinded to the allocated interventions for primary analyses.
O le numera o laina amata mo taunuʻuga muamua ma le lua o le a faʻaaogaina e faʻatusatusa ai le pulea ma le faʻamalosia o vaega. O fuainumera fuainumera faamaumauina o le a faia i luga o le faavae o le faamoemoe-ma-treat mataupu, o lona uiga o tagata maʻi o le a auiliiliina i le vaega o togafitiga lea na atofa i ai. I suʻesuʻega autū, o faʻamatalaga o loʻo misi o le a suia i le faigofie ma manino o le 'Baseline Observation Carred Forward' (BOCF), ma mo le lagona faʻapitoa foi o le a faʻaaogaina le tele o faʻaaogaina o faʻatulagaga.
Lona lua, ina ia faʻamatalaina taunuuga i le tausisia, o le a faʻaaogaina foi le 'per protocol' analysis. O le 'faasologa masani' o le faitau aofaʻi o tagata gasegase 'ua maeʻa' le gaioiga na tuʻuina atu ia i latou, e tusa ai ma taʻiala o loʻo faʻamatalaina i le vaega o loʻo i luga.
Mafaufauga Tino
Na talia e le Komiti Faʻatekonolosi Faʻasaienisi a le Itumalo o Tenimaka i Saute le suʻesuʻega (S-20100069). O le suʻesuʻega na faʻatusalia i le Tautinoga o Helsinki 2008 [47] e ala i le faʻataunuuina o fautuaga lautele lautele.
O mataupu uma lava o le a maua faʻamatalaga e uiga i le faʻamoemoe ma le anotusi o le poloketi ma tuʻuina atu a latou faʻatagaga tuusaʻo ma tusitusia e auai, faatasi ai ma le avanoa e faʻavae ai le poloketi i soʻo se taimi.
Dr. Alex Jimenez's Insight
O le puleaina o le atuatuvale, atuatuvale, atuatuvalega ma faailoga o le faaletonu o le misa, pe o le PTSD, pe a uma ona aafia i se faalavelave tau taavale e mafai ona faigata, aemaise lava pe afai o le mea na tupu na mafua ai le vevesi o le tino ma manuʻa pe faateteleina ai se tulaga oi ai nei. I le tele o tulaga, o lagona atuatuvale ma mafaufauga o mafaufauga na mafua mai i le faalavelave atonu o le punavai o faailoga tiga. I El Paso, TX, e toʻatele le au veterans ma le PTSD e asiasi i loʻu falemaʻi pe a uma ona faʻaalia le faʻaleagaina o faʻamaoniga mai se manua faʻafuaseʻi o se faalavelave faʻafuaseʻi. O le togafitiga faʻafeusuai e mafai ona tuʻuina atu ai i tagata maʻi le tatau lelei o le puleaina o le siosiomaga latou te manaʻomia e faʻaleleia ai o latou faʻafitauli faaletino ma faalelagona. E mafai foi e togafitiga faʻamaʻi togafitiga ona togafitia le tele o manuʻa faʻafuaseʻi faʻafuaseʻi, e aofia ai le afaina, le ulu ma le ua, manua ma le toe foi i tua.
Talanoaga
O lenei suʻesuʻega o le a fesoasoani i se malamalama sili atu i le togafitia o tagata gasegase i le faʻavaʻa o le ua i le maeʻa ai o se faʻalavelave lavelave. O le malamalama mai lenei suʻesuʻega e mafai ona faʻatinoina i le faʻatinoga faʻapitoa, ona o le suʻesuʻega e faʻavaeina i luga o auala e tele, e faʻatusatusa i le auala, e ui lava i le leai o se faʻamaoniga, e masani lava ona faʻaaogaina i se togafitiga o le physiotherapy. O le suʻesuʻega e mafai foi ona aofia i iloiloga faʻalauteleina e ala i le saofaga i le faʻafouina o le malamalama e uiga i lenei faitau aofaʻi ma le faʻaleleia o togafitiga faʻavae molimau.
Faʻasalalau le mamanu o se suʻesuʻega aʻo leʻi faia le suʻesuʻega ma o le a maua ai le tele o faʻamanuiaga e maua mai. E mafai ai ona faʻamaeʻaina le mamanu e aunoa ma lona aʻafiaina i taunuʻuga. O lenei mea e mafai ona fesoasoani i le puipuia o le faʻaituau e pei o mea sese mai le uluai mamanu e mafai ona iloa. O isi suʻesuʻega suʻesuʻega o le a maua ai le avanoa e mulimuli ai i se auala talitutusa e tusa ai ma le faitau aofaʻi, faʻasalalauga, taʻiala ma fuataga. O luitau o lenei suʻesuʻega e fesoʻotaʻi ma le faʻamaoniaina o faʻasalalauga, togafitiga o le faitau aofai e le tutusa, faʻamalamalamaina ma faʻatulagaina fuafaatatau talafeagai i luga o le faitau aofaʻi o faʻamaʻi tumau ma maua ai le faitau aofaʻi mai nofoaga eseese e lua. O le faʻamaoniaina o faʻasalalauga e maua mai e ala i le aʻoaʻoina o le fomaʻi o loʻo aʻafia i totonu o se aʻoaʻoga. O le tutusa o le faitau aofaʻi o tagata o le a faʻafoeina e ala i le tuʻufaʻatasia ma le faʻaaogaina o faʻataʻitaʻiga ma le mataʻituina o uiga o tagata gasegase, ma le eseesega i le va o vaega e faʻavae i luga o isi aʻafiaga nai lo le faʻataʻitaʻiina / pulea o le a mafai ona suʻe fuainumera. O lenei mamanu suʻesuʻega ua aofia ai o se 'faʻaopoopoga' mamanu: o vaega uma e lua e maua aʻoaʻoga o le tiga; o le vaega faʻasosolo e faʻaopoopoina aʻoaʻoga faʻapitoa, e aofia ai faʻamalosi faapitoa o le tino ma aʻoaʻoga lautele. I aso nei e le lava molimau mo le aʻafiaga o le togafitiga mo tagata gasegase e tigaina le tiga o le ua i le maea ai o se faʻalavelave lavelave. O tagata uma o loʻo auai o le a tuʻuina atu mo se togafitiga (faʻataʻitaʻiina poʻo le faʻaosoosoina), aua tatou te manatu e le faʻamalosi e le ofoina atu nisi ituaiga o togafitiga, e pei o le faʻasagaina o le kulupu pule i se lisi faʻatali. O le faʻaopoopoga o mamanu ua filifilia e avea o se fofo faʻaaoga lelei i se tulaga faapena [48].
For whiplash patients with chronic pain, the most responsive disability measures (for the individual patient, not for the group as a whole) are considered to be the Patient Specific Functional Scale and the numerical rating scale of pain bothersomeness [49]. By using these and NDI (the most often used neck disability measure) as secondary outcome measures, it is anticipated that patient-relevant changes in pain and disability can be evaluated. The population will be recruited from and treated at two different clinical settings: the out-patient clinic of The Spine Centre, Hospital Lilleb�lt and several private physiotherapy clinics. To avoid any influence of the different settings on the outcome measures, the population will be block randomised related to the settings, securing equal distribution of participants from each setting to the two intervention groups.
Faʻateleina Tauiloa
Fai mai tusitala e leai ni a latou tauvaga.
Fesoasoani a Tagata Tusitala
Na tusia e le IRH ia tusitusiga. IRH, BJK ma KS na auai i le mamanu o le suʻesuʻega. Na saofagā uma i le mamanu. RC, IRH; Na auai le BJK ma le KS i le malosiaga ma le faataʻitaʻiga o le tele o fuainumera ma i le faamatalaina o le auiliiliga o fuainumera faamaumauina faapea foi ma le faasoasoaina ma le faasologa o taualumaga. O tusitala uma na faitauina ma faamaonia le tusitusiga mulimuli. Sa saunia e Suzanne Capell le fesoasoani tusitusi ma faasaʻo le gagana.
Pre-Publication History
O le faʻasalalauga faʻasalalau mo lenei pepa e mafai ona maua iinei: www.biomedcentral.com/1471-2474/12/274/prepub
Faʻafetai
O lenei suʻesuʻega na maua ai le faʻatupega mai le Research Fund mo le Itumalo o Tenimaka i Saute, le Faalapotopotoga o Rheumatism Danimaka, le Research Foundation o le Faalapotopotoga a le Danish Association of Physiotherapy, o le Faaputugatupe mo le Vailaau Faʻatekonolosi i Faiga Faʻapitoa, ma le Danish Society of Polio and Victims Victims (PTU). ). Ole Vaega o Fuainumera Faamaumauina i le Parker Institute e lagolagoina e fesoasoani mai le Oak Foundation. Sa saunia e Suzanne Capell le fesoasoani tusitusi ma le faʻaaogaina o gagana.
Ua faamauina le faamasinoga www.ClinicalTrials.gov e faailoa NCT01431261.
O le Faʻatonuina o le Faʻataʻitaʻiina o Faʻamatalaga Faʻamalosi-Faʻasalalauga mo le togafitia o le PTSD i le anotusi o Chronic Whiplash
lē faʻatino
sini
O faʻamaʻi pipisi o le vaʻaia (WAD) e taatele ma aofia ai faʻaletonu faaletino ma le mafaufau. Ua faʻaalia e le suʻesuʻega o faʻamalosiaga faʻasolosolo faʻasalaga e fesoʻotaʻi ma le toe faʻafoʻisia o galuega ma le faʻaleleia o le tino. O le togafitiga o le mafaufau-amioga-togafitiga (TF-CBT) ua faʻaalia ai le aoga lelei i faʻasologa o tiga o taimi masani. Ae ui i lea, e oʻo mai i le taimi nei, e leai ni faʻamasinoga faʻapitoa i totonu o le WAD. O lea la, o lenei suʻesuʻega o le a lipotia ai le aoga o le TF-CBT i tagata taʻitasi e faʻafetaui le taʻiala mo le WAD masani ma le posttraumatic stress disorder (PTSD).
faiga
E lua sefulu ono tagata auai na tofiaina i le TF-CBT poʻo le faʻatonuga o le faʻatali, ma na iloiloina togafitiga i togafitiga ma le mulimulitaia o le 6 i le faʻaaogaina o se faʻatalanoaga o le falemaʻi, suʻega a le tagata lava ia, ma fuataga o le tiga o le tino ma le lagona faimalaga.
i'uga
Ole faʻaitiitia o faʻamaʻi ile faʻafitauli ile PTSD i le vaega ole TF-CBT pe a faatusatusa i le tagata faatalitali i le maeʻa, ma isi faʻamatalaga na matauina i le tulitatao. O le togafitiga o le PTSD na faʻapipiʻiina foi ma le faʻaleleia atili o le malosi o le ua, le tino, lagona, ma le agafesoʻotaʻi ma le faʻafoʻiina o le tino i faʻamaʻi, ae o suiga laiti na maua i le faʻailoga tiga.
Talanoaga
O lenei suʻesuʻega e maua ai le lagolago mo le aoga o le TF-CBT ina ia faʻataʻitaʻiina ai faailoga o le PTSD i totonu o le WAD masani. O le mauaina o le togafitiga o le PTSD na mafua ai le faaleleia o le le atoatoa o le ua ma le lelei o le olaga ma suiga i le tulaga o le tiga o le vevela ua faamaninoina ai le faigata ma le vavalalataina o auala e maua uma ai le WAD ma le PTSD. O aʻafiaga o suʻesuʻega o suʻesuʻega ma faʻataʻitaʻiga o le lumanaʻi e talanoaina.
I le faaiuga, o le aafia ai i se faalavelave faʻafuaseʻi tau taavale o se tulaga e le manaʻomia lea e mafai ona mafua ai le tele o faʻalavelave faʻaleagaina poʻo manuaga faʻapea foi i le atinaʻeina o le tele o tulaga faʻateteleina. Ae ui i lea, o le atuatuvale, atuatuvalega, atuatuvale ma le afaina o le le mautonu, po o le PTSD, o faafitauli masani o le mafaufau e ono tulai mai o se taunuuga o se faalavelave tau taavale. E tusa ai ma suʻesuʻega suʻesuʻega, o aʻafiaga faaletino ma mafatiaga faʻalagona e mafai ona vavalalata vavalalata ma togafitiga faʻaleagaga faaletino ma faalelagona e mafai ona fesoasoani i tagata gasegase ia ausia le soifua maloloina ma le soifua lelei. Faʻamatalaga mai le National Center for Biotechnology Information (NCBI). O le lautele o a tatou faʻamatalaga e faʻapulaʻaina i le faʻamaʻi faʻamaʻi faʻapea foi ma manua ma tuʻutuʻu. Ina ia talanoaina le mataupu, faamolemole ia lagona le saoloto e fesili atu ia Dr. Jimenez pe faʻafesoʻotaʻi mai i matou 915-850-0900 .
Faʻailoina e Dr. Alex Jimenez
Aʻoaʻoga Faʻaopoopo: Paʻu Paʻa
E tusa ai ma fuainumera, e tusa ma le 80% o tagata o le a oʻo i faʻamaoniga o tiga i tua e le itiiti ifo ma le tasi i o latou olaga atoa. Paʻu tua o se faasea masani lea e mafai ona mafua ona o le tele o manuʻa ma / poʻo tuutuuga. O le tele o taimi, o le faʻaleagaina masani o le vaʻai ma le matutua e ono mafua ai le tiga. Faiga faʻamaʻi e tupu pe a tuleia le nofoaga tutotonu, pei o le gel o se pusa faʻafefefebral e ala i se loimata i lona taamilosaga, pito i fafo o le cartilage, faʻamalosi ma faʻafefe ai aʻa aʻa. O faʻasalaga faʻasalalau e masani lava ona tutupu i le pito i lalo, poʻo le lumine spine, ae e mafai foi ona tupu i luga o le tui o le au, poo le ua. O le afaina o neura e maua i le maualalo ona o le manua ma / poʻo se tulaga faʻateleina e mafai ona oʻo atu ai i faailoga o le sciatica.

TULAGA FAATINO TUSI: Puleaina o le Nofoaga Faʻanoanoa
TALI FAATINO AUTU: FAʻAALIGA FAʻAALIGA: Taʻaloga o le Manuaga Faʻafuaseʻi El Paso, TX Chiropractor
Blank
mau faasino
1. Le National Institute of Public H. Folkesundhedsrapporten, 2007 (aofia: Lipoti a le Soifua Maloloina, Tenimaka, 2007) 2007. ps112.
2. Whiplash kommisionen och Svenska Lkl. Diagnostik och tidigt omh�ndertagande av whiplashskador (engl: Diagnostics and early treatment of Whiplash Injuries) Sandviken: Sandvikens tryckeri; 2005.
3. Carroll LJ, Hogg-Johnson S, van dV, Haldeman S, Holm LW, Carragee EJ, Hurwitz EL, Cote P, Nordin M, Peloso PM. et al. Course and prognostic factors for neck pain in the general population: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine. 2008;12(4 Suppl):S75�S82. [PubMed]
4. Nijs J, Oosterwijck van J, Hertogh de W. Rehabilitation of chronic whiplash: treatment of cervical dysfunctions or chronic pain syndrome? ClinRheumatol. 2009;12(3):243�251. [PubMed]
5. Falla D. Unravelling the complexity of muscle impairment in chronic neck pain. ManTher. 2004;12(3):125�133. [PubMed]
6. Mannerkorpi K, Henriksson C. Non-pharmacological treatment of chronic widespread musculoskeletal pain. BestPractResClinRheumatol. 2007;12(3):513�534. [PubMed]
7. Kay TM, Maea A, Goldsmith C, Santaguida PL, Tiliina o J, Bronfort G. Gaioiga mo faaletonu o le ua. CochraneDatabaseSystRev. 2005. p. CD004250. [PubMed]
8. Kasch H, Qerama E, Kongsted A, Bendix T, Jensen TS, Bach FW. Clinical assessment of prognostic factors for long-term pain and handicap after whiplash injury: a 1-year prospective study. EurJNeurol. 2008;12(11):1222�1230. [PubMed]
9. Curatolo M, Arendt-Nielsen L, Petersen-Felix S. Central hypersensitivity in chronic pain: mechanisms and clinical implications. PhysMedRehabilClinNAm. 2006;12(2):287�302. [PubMed]
10. Jull G, Sterling M, Kenardy J, Beller E. Does the presence of sensory hypersensitivity influence outcomes of physical rehabilitation for chronic whiplash?–A preliminary RCT. Pain. 2007;12(1-2):28�34. doi: 10.1016/j.pain.2006.09.030. [PubMed] [Cross Ref]
11. Davis C. Chronic pain/dysfunction in whiplash-associated disorders95. JManipulative Physiol Ther. 2001;12(1):44�51. doi: 10.1067/mmt.2001.112012. [PubMed] [Cross Ref]
12. Flor H. Cortical reorganisation and chronic pain: implications for rehabilitation. JRehabilMed. 2003. pp. 66�72. [PubMed]
13. Bosma FK, Kessels RP. Cognitive impairments, psychological dysfunction, and coping styles in patients with chronic whiplash syndrome14. Neuropsychiatry NeuropsycholBehavNeurol. 2002;12(1):56�65. [PubMed]
14. Guez M. Chronic tiga o le ua. O suʻesuʻega faʻamaʻi, mafaufau ma mafaufauga faʻatasi ma le faʻamalosi i faʻamaʻi pipisi e fesoʻotaʻi faʻamaʻi pipisi9. Acta OrthopSuppl. 2006; 12 (320): toe faʻaleleia-33. [PubMed]
15. Kessels RP, Aleman A, Verhagen WI, van Luijtelaar EL. Cognitive functioning after whiplash injury: a meta-analysis5. JIntNeuropsycholSoc. 2000;12(3):271�278. [PubMed]
16. O’Sullivan PB. Lumbar segmental ‘instability’: clinical presentation and specific stabilizing exercise management. ManTher. 2000;12(1):2�12. [PubMed]
17. Jull G, Falla D, Treleaven J, Hodges P, Vicenzino B. Retraining cervical joint position sense: the effect of two exercise regimes. JOrthopRes. 2007;12(3):404�412. [PubMed]
18. Falla D, Jull G, Hodges P, Vicenzino B. An endurance-strength training regime is effective in reducing myoelectric manifestations of cervical flexor muscle fatigue in females with chronic neck pain. ClinNeurophysiol. 2006;12(4):828�837. [PubMed]
19. Gill JR, Brown CA. A structured review of the evidence for pacing as a chronic pain intervention. EurJPain. 2009;12(2):214�216. [PubMed]
20. Wallman KE, Morton AR, Goodman C, Grove R, Guilfoyle AM. Randomised controlled trial of graded exercise in chronic fatigue syndrome. MedJAust. 2004;12(9):444�448. [PubMed]
21. Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: model, processes and outcomes. BehavResTher. 2006;12(1):1�25. [PubMed]
22. Lappalainen R, Lehtonen T, Skarp E, Taubert E, Ojanen M, Hayes SC. The impact of CBT and ACT models using psychology trainee therapists: a preliminary controlled effectiveness trial. BehavModif. 2007;12(4):488�511. [PubMed]
23. Linton SJ, Andersson T. Can chronic disability be prevented? A randomized trial of a cognitive-behavior intervention and two forms of information for patients with spinal pain. Spine (Phila Pa 1976) 2000;12(21):2825�2831. doi: 10.1097/00007632-200011010-00017. [PubMed] [Cross Ref]
24. Moseley L. Combined physiotherapy and education is efficacious for chronic low back pain. AustJPhysiother. 2002;12(4):297�302. [PubMed]
25. Soderlund A, Lindberg P. Cognitive behavioural components in physiotherapy management of chronic whiplash associated disorders (WAD)–a randomised group study6. GItalMedLavErgon. 2007;12(1 Suppl A):A5�11. [PubMed]
26. Wicksell RK. Faʻaalia ma le taliaina i tagata gasegase e maua ai le tiga matuitui - o se faʻataʻitaʻiga faʻataʻitaʻiga e faʻaleleia ai le galue ma le lelei o le olaga. Karolinska Institutet; 2009.
27. Seferiadis A, Rosenfeld M, Gunnarsson R. A review of treatment interventions in whiplash-associated disorders70. EurSpine J. 2004;12(5):387�397. [PMC free article] [PubMed]
28. van der Wees PJ, Jamtvedt G, Rebbeck T, de Bie RA, Dekker J, Hendriks EJ. Multifaceted strategies may increase implementation of physiotherapy clinical guidelines: a systematic review. AustJPhysiother. 2008;12(4):233�241. [PubMed]
29. Verhagen AP, Scholten-Peeters GG, van WS, de Bie RA, Bierma-Zeinstra SM. Faʻatau togafitiga mo le whiplash34. CochraneDatabaseSystRev. 2009. p. CD003338.
30. Hurwitz EL, Carragee EJ, van dV, Carroll LJ, Nordin M, Guzman J, Peloso PM, Holm LW, Cote P, Hogg-Johnson S. et al. Treatment of neck pain: noninvasive interventions: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine. 2008;12(4 Suppl):S123�S152. [PubMed]
31. Stewart MJ, Maher CG, Refshauge KM, Herbert RD, Bogduk N, Nicholas M. Randomized controlled trial of exercise for chronic whiplash-associated disorders. Pain. 2007;12(1-2):59�68. doi: 10.1016/j.pain.2006.08.030. [PubMed] [Cross Ref]
32. Ask T, Strand LI, Sture SJ. The effect of two exercise regimes; motor control versus endurance/strength training for patients with whiplash-associated disorders: a randomized controlled pilot study. ClinRehabil. 2009;12(9):812�823. [PubMed]
33. Rubinstein SM, Pool JJ, van Tulder MW, Riphagen II, de Vet HC. A systematic review of the diagnostic accuracy of provocative tests of the neck for diagnosing cervical radiculopathy. EurSpine J. 2007;12(3):307�319. [PMC free article] [PubMed]
34. Peolsson M, Borsbo B, Gerdle B. Generalized pain is associated with more negative consequences than local or regional pain: a study of chronic whiplash-associated disorders7. JRehabilMed. 2007;12(3):260�268. [PubMed]
35. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. ArchGenPsychiatry. 1961;12:561�571. [PubMed]
36. Wicksell RK, Ahlqvist J, Bring A, Melin L, Olsson GL. Can exposure and acceptance strategies improve functioning and life satisfaction in people with chronic pain and whiplash-associated disorders (WAD)? A randomized controlled trial. Cogn BehavTher. 2008;12(3):169�182. [PubMed]
37. Falla D, Jull G, Dall’Alba P, Rainoldi A, Merletti R. An electromyographic analysis of the deep cervical flexor muscles in performance of craniocervical flexion. PhysTher. 2003;12(10):899�906. [PubMed]
38. Palmgren PJ, Sandstrom PJ, Lundqvist FJ, Heikkila H. Improvement after chiropractic care in cervicocephalic kinesthetic sensibility and subjective pain intensity in patients with nontraumatic chronic neck pain. JManipulative Physiol Ther. 2006;12(2):100�106. doi: 10.1016/j.jmpt.2005.12.002. [PubMed] [Cross Ref]
39. Borg G. Psychophysical scaling with applications in physical work and the perception of exertion. ScandJWork EnvironHealth. 1990;12(Suppl 1):55�58. [PubMed]
40. Wallman KE, Morton AR, Goodman C, Grove R. Exercise prescription for individuals with chronic fatigue syndrome. MedJAust. 2005;12(3):142�143. [PubMed]
41. McCarthy MJ, Grevitt MP, Silcocks P, Hobbs G. The reliability of the Vernon and Mior neck disability index, and its validity compared with the short form-36 health survey questionnaire. EurSpine J. 2007;12(12):2111�2117. [PMC free article] [PubMed]
42. Bjorner JB, Damsgaard MT, Watt T, Groenvold M. Tests of data quality, scaling assumptions, and reliability of the Danish SF-36. JClinEpidemiol. 1998;12(11):1001�1011. [PubMed]
43. Ware JE Jr, Kosinski M, Bayliss MS, McHorney CA, Rogers WH, Raczek A. Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. MedCare. 1995;12(4 Suppl):AS264�AS279. [PubMed]
44. Ware JE Jr. SF-36 health survey update. Spine (Phila Pa 1976) 2000;12(24):3130�3139. doi: 10.1097/00007632-200012150-00008. [PubMed] [Cross Ref]
45. Carreon LY, Glassman SD, Campbell MJ, Anderson PA. Le Disability Index, puʻupuʻu-36 tino vaega otootoga, ma fua una mo ua ma lima tiga: le maualalo falemaʻi taua eseesega ma tele aoga faʻamanuiaga pe a maeʻa faʻafaʻa tuʻufaʻatasiga o le faʻaautagata. Spine J. 2010; 12 (6): 469--474. fai: 10.1016 / j.spinee.2010.02.007. [Faʻasalalau] [Cross Ref]
46. Moher D, Hopewell S, Schulz KF, Montori V, Gotzsche PC, Devereaux PJ, Elbourne D, Egger M, Altman DG. CONSORT 2010 Explanation and Elaboration: Updated guidelines for reporting parallel group randomised trials. JClinEpidemiol. 2010;12(8):e1�37. [PubMed]
47. Mataupu WDoH-EPfMRIH. FUAFUAGA A LE LALOLAGI O LE LALOLAGI O LE HELSINKI. Folafolaga a le WMA o Helsinki - Taʻiala Faʻavae mo Suʻesuʻega Faʻataʻitaʻiga Faʻaaofia Tagata Tagata. 2008.
48. Dworkin RH, Turk DC, Peirce-Sandner S, Baron R, Bellamy N, Burke LB, Chappell A, Chartier K, Cleeland CS, Costello A. et al. Research design considerations for confirmatory chronic pain clinical trials: IMMPACT recommendations. Pain. 2010;12(2):177�193. doi: 10.1016/j.pain.2010.02.018. [PubMed] [Cross Ref]
49. Stewart M, Maher CG, Refshauge KM, Bogduk N, Nicholas M. Responsiveness of pain and disability measures for chronic whiplash. Spine (Phila Pa 1976) 2007;12(5):580�585. doi: 10.1097/01.brs.0000256380.71056.6d. [PubMed] [Cross Ref]
50. Jull GA, O’Leary SP, Falla DL. Clinical assessment of the deep cervical flexor muscles: the craniocervical flexion test. JManipulative Physiol Ther. 2008;12(7):525�533. doi: 10.1016/j.jmpt.2008.08.003. [PubMed] [Cross Ref]
51. Revel M, Minguet M, Gregoy P, Vaillant J, Manuel JL. Changes in cervicocephalic kinesthesia after a proprioceptive rehabilitation program in patients with neck pain: a randomized controlled study. ArchPhysMedRehabil. 1994;12(8):895�899. [PubMed]
52. Heikkila HV, Wenngren BI. Cervicocephalic kinesthetic sensibility, active range of cervical motion, and oculomotor function in patients with whiplash injury. ArchPhysMedRehabil. 1998;12(9):1089�1094. [PubMed]
53. Treleaven J, Jull G, Grip H. Vaʻavaʻa mata ma vaʻavaʻai i le faʻamautuina i mataupu ei ai faʻamaʻi pipisi e fesoʻotaʻi faʻatasi. Man Ther. 2010. [PubMed]
54. Williams MA, McCarthy CJ, Chorti A, Cooke MW, Gates S. A systematic review of reliability and validity studies of methods for measuring active and passive cervical range of motion. JManipulative Physiol Ther. 2010;12(2):138�155. doi: 10.1016/j.jmpt.2009.12.009. [PubMed] [Cross Ref]
55. Kasch H, Qerama E, Kongsted A, Bach FW, Bendix T, Jensen TS. Deep muscle pain, tender points and recovery in acute whiplash patients: a 1-year follow-up study. Pain. 2008;12(1):65�73. doi: 10.1016/j.pain.2008.07.008. [PubMed] [Cross Ref]
56. Sterling M. Testing for sensory hypersensitivity or central hyperexcitability associated with cervical spine pain. JManipulative Physiol Ther. 2008;12(7):534�539. doi: 10.1016/j.jmpt.2008.08.002. [PubMed] [Cross Ref]
57. Ettlin T, Schuster C, Stoffel R, Bruderlin A, Kischka U. A distinct pattern of myofascial findings in patients after whiplash injury. ArchPhysMedRehabil. 2008;12(7):1290�1293. [PubMed]
58. Vernon H, Mior S. The Neck Disability Index: a study of reliability and validity. JManipulative Physiol Ther. 1991;12(7):409�415. [PubMed]
59. Vernon H. The Neck Disability Index: state-of-the-art, 1991-2008. JManipulative Physiol Ther. 2008;12(7):491�502. doi: 10.1016/j.jmpt.2008.08.006. [PubMed] [Cross Ref]
60. Vernon H, Guerriero R, Kavanaugh S, Soave D, Moreton J. Psychological factors in the use of the neck disability index in chronic whiplash patients. Spine (Phila Pa 1976) 2010;12(1):E16�E21. doi: 10.1097/BRS.0b013e3181b135aa. [PubMed] [Cross Ref]
61. Sterling M, Kenardy J, Jull G, Vicenzino B. The development of psychological changes following whiplash injury. Pain. 2003;12(3):481�489. doi: 10.1016/j.pain.2003.09.013. [PubMed] [Cross Ref]
62. Stalnacke BM. Relationship between symptoms and psychological factors five years after whiplash injury. JRehabilMed. 2009;12(5):353�359. [PubMed]
63. Rabin R, de CF. EQ-5D: a measure of health status from the EuroQol Group. AnnMed. 2001;12(5):337�343. [PubMed]
64. Borsbo B, Peolsson M, Gerdle B. Catastrophizing, depression, and pain: correlation with and influence on quality of life and health – a study of chronic whiplash-associated disorders4. JRehabilMed. 2008;12(7):562�569. [PubMed]