Versebral Artery Dissection Na Maua I le taimi o le Suʻega Chiropractic
Acknowledging the subsequent information below,�pe tusa ma le 2 miliona tagata ua manua i faalavelave tau taavale i tausaga taʻitasi ma i na mea na tupu, o le toʻatele o tagata o aafia ai e maua i le lavelave ma / poʻo le faʻamaʻi o le ua ile tausi maʻi. A oʻo i le faʻalavelave faʻalavelave o le ua faʻavaivai, faʻaleagaina le tino ma isi faʻafitauli faafomaʻi atonu e tupu. Versebral arse dissection, poʻo le VAD, o loʻo faʻaalia i se loimata e pei o le loimata i totonu o le faʻaoʻo totonu o le vete vertebral e nafa ma le tuʻuina atu o le toto i le faiʻai. A mavae le loimata, ona mafai lea e le toto ona ulufale i le puipui o le pa ma fausia ai se toto toto, faʻamalo le puipui o le faʻamalo ma masani ona faʻafefe toto.
Through years of experience practicing chiropractic care,�VAD may often follow after trauma to the neck, such as that which occurs in an automobile accident, or whiplash injury. The symptoms of vertebral artery dissection include head and neck pain as well as intermittent or permanent stroke symptoms, such as difficulty speaking, impaired coordination and loss of vision. VAD, or vertebral artery dissection, is generally diagnosed with a contrast-enhanced CT or MRI scan.
lē faʻatino
O se tina 30 tausaga le matua na tuuina atu i se matagaluega o faalavelave faafuaseʻi ma le faafuaseʻi o le amataina o le tumau leiloa o le tauagavale peripheral vaʻai. Ona o le tala faasolopito o le ulu o le ulu, na faasaolotoina ai o ia ma le siama o le ovular migraine. Lua aso mulimuli ane, na ia sailia togafitiga o le fomaʻi mo le faʻailoga sili o le tiga o le ua. Na masalomia e le fomai togafiti le ono iai se vavaeese o le alatoto (VAD). Leai se togafiti faʻataʻitaʻi; nai lo lena, MR angiography (MRA) o le ua na mauaina, lea na faʻaalia ai se tiga agavale VAD ma vave thrombus faʻavae. O le tagata gasegase na tuu i luga o le aspirin togafitiga. Toe fai le MRA o le ua 3 masina mulimuli ane faʻailoa mai le iʻuga o le thrombus, e aunoa ma le faʻaauau i le stroke. O lenei mataupu o loʻo atagia mai ai le taua mo tausi soifua maloloina uma o loʻo vaʻaia tagata mamaʻi ma le tiga o le ua ma le ulu tiga o le uaʻi ina ia mataala i le faʻaaliga faʻailoaina o le ono VAD o loʻo agaʻi i luma.
tua
Vertebral artery dissection (VAD) e tau atu i le stroke o se mea e le masani ai ae ono oʻo i se faʻamaʻi faigata. Ole faʻalavelave ole stroke e faʻatatau ile vertebrobasilar system e ese mai ile 0.75 ile 1.12 / 100? 000 tagata-tausaga. O le pathological taualumaga i VAD masani aofia ai dissection o le pa o le alatoto mulimuli ane i se taimi mulimuli ane e thrombus fausiaina, lea e ono mafua ai arterial occlud pe ono taitai atu ai i embolisation, mafua ai occlud o se tasi po o le sili atu o le distal lala mai le vertebral alatoto, aofia ai le basilar alatoto, lea e mafai ona afaina ai. E masani ona tupu le VAD i tagata mamaʻi o loʻo iai se vaivaiga masani, e le tumau ile pa puipui. I le tusa o le 80% o mataupu, o uluaʻi faʻailoga e aofia ai le tiga o le ua ma pe leai le tiga o le ulu.
Many patients with VAD may in the early stages present to chiropractors seeking relief from neck pain and headache, without realising they are experiencing VAD. In many of these cases, the patient later develops a stroke. Until recently, it was assumed that the dissection (and subsequent stroke) was caused by cervical manipulative therapy (CMT). However, while early studies found an association between visits to a chiropractor and subsequent stroke related to VAD, recent data suggest that this relationship is not causal.
O lenei lipoti o le faʻataʻitaʻiga lea o le faʻataʻitaʻiga lea na faʻatautaia ai e le tagata maʻi se VAD e leʻi faʻaalia i le evolusione se faʻataʻitaʻiga mo le tiga o le ua ma le ulu. Ina ua maeʻa le talaaga ma le suʻesuʻega, na masalomia e le tagata vavalo le VAD ma e leʻi faia CMT. Nai lo lena, na tuʻuina atu le tagata gasegase mo isi suʻesuʻega, lea na faʻamaonia ai le agai i luma o le VAD. O togafitiga faʻafuaseʻi ma togafitiga faʻapitoa o togafitiga na manatu e ono faʻagasolo ai le alualu i luma i le paʻu.
Tulaga Faʻaalia
A 30-year-old otherwise healthy woman consulted a chiropractor (DBF), reporting of right-sided neck pain in the suboccipital region. The patient reported that, 3?days previously, she had gone to the local hospital emergency department (ED) because of the sudden onset of loss of left peripheral vision. The visual symptoms interfered with her ability to see through her left eye; this was accompanied by �numbness� in her left eyelid. About 2?weeks prior to this ED visit, she had experienced an episode of acute left-sided neck pain with severe left-sided headache. She also related a history of migraine headache without prodrome. She was released from the ED with a tentative diagnosis of ocular migraine. She had never been previously diagnosed with ocular migraine, nor had she ever experienced any visual disturbances with her previous migraines.
Shortly after the left-sided ocular symptoms resolved, she suddenly developed right-sided neck pain without provocation, for which she sought chiropractic treatment. She also reported a transient episode of right-sided visual disturbance occurring that same day as well. This was described as sudden blurriness that was of short duration and resolved spontaneously earlier in the day of her presentation for chiropractic examination. When she presented for the initial chiropractic examination, she denied current visual disturbance. She said that she was not experiencing any numbness, paraesthesia or motor loss in the upper or lower extremities. She denied ataxia or difficulty with balance. Medical history was remarkable for childbirth 2� months prior to initial presentation. She stated that her migraine headaches were associated with her menstrual cycle. Family history was remarkable for a spontaneous ascending thoracic aortic aneurysm in her older sister, who was about 30?years of age when her aneurysm had occurred.
Suʻesuʻega
Based on the history of sudden onset of severe upper cervical pain and headache with visual disturbance and ocular numbness, the DC was concerned about the possibility of early VAD. Urgent MR angiography (MRA) of the neck and head, along with MRI of the head, was ordered. No cervical spine examination or manipulation was performed because of the suspicion that the neck pain was related to VAD rather than to a �mechanical� cervical disorder.
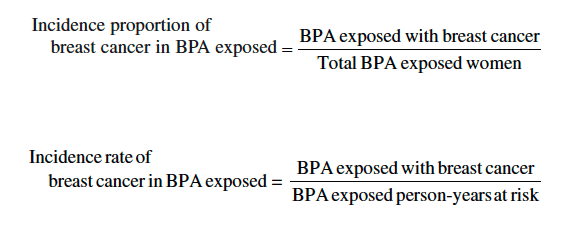
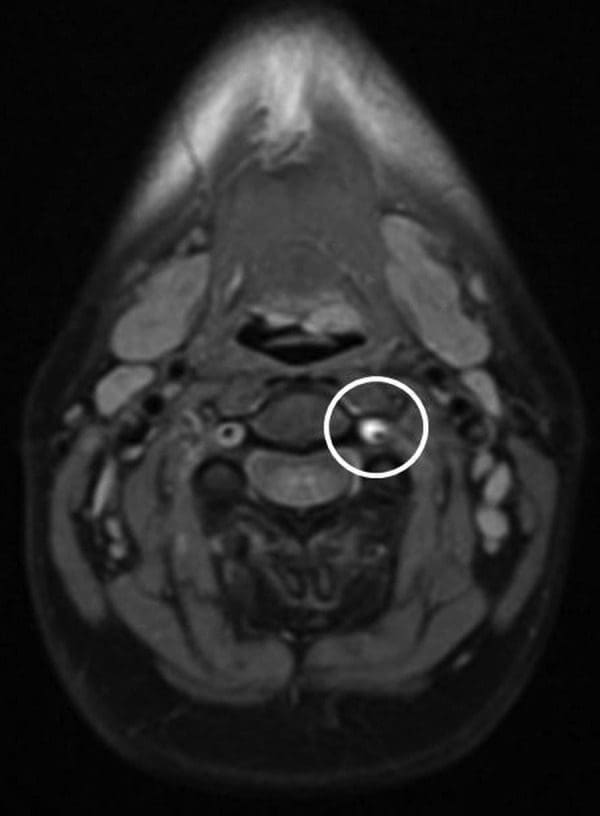
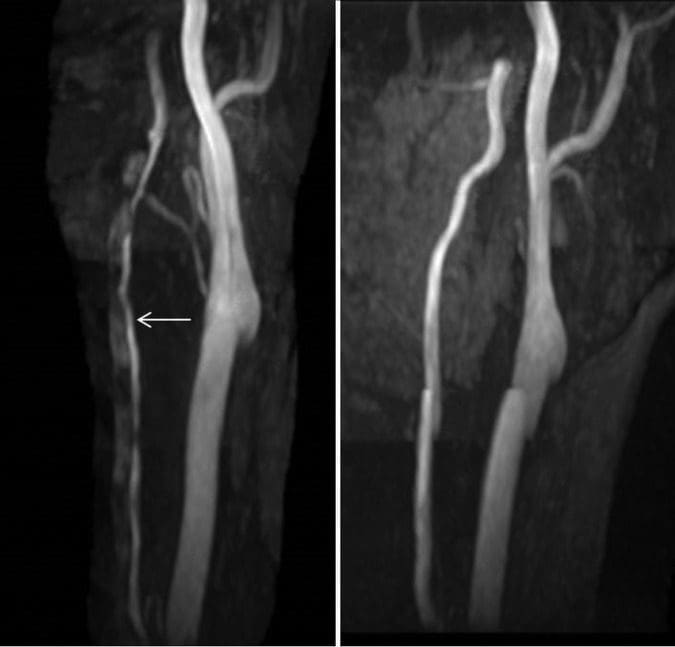
MRA o le ua faʻaalia o le agavale vertebral artery e laʻititi ma e le masani ai i le caliber, alu atu mai le C7 level cephalad i le C2, ogatasi ma dissection. Sa i ai le pateni moni lumen ma se siʻomia cuff o T1 hyper-malosi, ogatasi ma dissection ma subintimal thrombus i totonu o le sese lumen (Ata 1 ma? 2). MRI o le ulu ma aunoa ma le faʻatusatusaga, ma le MRA o le ulu e aunoa ma le faʻatusatusaina, sa le mafaamatalaina uma. Faʻapitoa lava, e leai se intracranial faʻalautelega o dissection poʻo faʻamaoniga o infarction. MR perfusion o le faiʻai na faʻaalia e leai ni mea faʻapitoa e faʻatumu ai ni vailaʻau.
Ata 1: O le maualuga o le ata o le faʻasolosolo o le ata e faʻaalia ai le maualuga o le maualuga o le gaʻo o loʻo siomia ai le ogaoga o le vertebral o loʻo totoe (e fai ma sui o le lumenise leaga). Manatua na faʻaitiitia le faʻamaʻi o le lumenia moni (faʻaaogaina le lanu uliuli) e tusa ai ma le aluga saʻo o le vertebral.
Ata 2: O foliga le talafeagai mai le tolu-taimi-time-flight MRA o loʻo faʻaalia ai le vaʻaia o le hypotense T1 e vavaeeseina ai le lumen moni (lautele) mai le lumenia lumine (medial). MRA, MR faʻamatalaga.
Eseesega Faʻamatalaga
The ED released the patient with a tentative diagnosis of ocular migraine, due to her history of migraine headaches. However, the patient stated that the left-sided headache was atypical��like nothing I’ve ever experienced before.� Her previous migraines were associated with her menstrual cycle, but not with any vision changes. She had never been previously diagnosed with ocular migraine. MRA of the cervical region revealed that the patient actually had an acute dissection with thrombus formation in the left vertebral artery.
faiga
Owing to the potential of impending stroke associated with an acute VAD with thrombus formation, the patient was admitted to the neurology stroke service for close neurological monitoring. During her admission, the patient did not experience any recurrence of neurological deficits and her headaches improved. She was discharged the following day with a diagnosis of left VAD and transient ischaemic attack. She was instructed to avoid vigorous exercise and trauma to the neck. Daily aspirin (325?mg) was prescribed, to be continued for 3�6?months after discharge.
Taunuuga ma Tulitatao
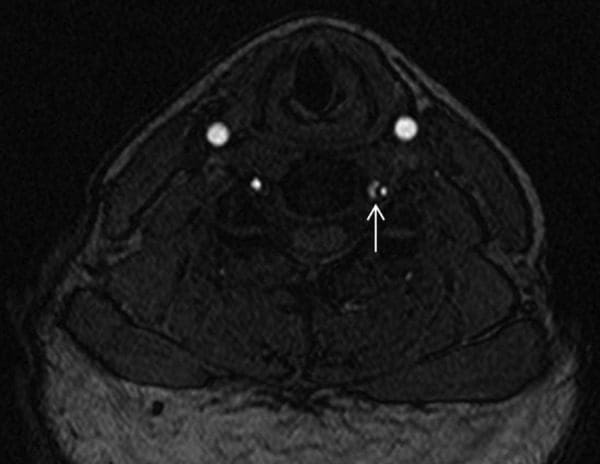
Ina ua maeʻa ona faʻateʻaina mai le tautua a le stroke, sa leai se toe oso o le tiga o le ulu poʻo ni faʻalavelave faʻafuaseʻi, ma o ona tua tua tiga tiga na faʻamaonia. Faʻaauau ata na faia 3? Masina ina ua maeʻa le faʻaliga, lea na faʻaalia ai le faʻaleleia o le kalama o le ua o le cerular left vertebral arter ma le iugafono o le thrombus i totonu o le lumen sese (Ata 3). Faʻataʻitaʻiga o le potu i totonu o le fale na tumau pea le masani, e aunoa ma le faʻamaonia o le vaitaimi infarction poʻo le perfusion asymmetry.
Ata 3: Malosiaga maualuga maualuga (MIP) ata mai le tolu-taimi-taimi o le MRA (o le agavale taua o le taimi o le faʻaaliga ma le ata saʻo o le 3 masina mulimuli). O le ata muamua o loʻo faʻaalia ai le faasolosolo malie o le pito i luga o le alatoto o le vertebral
Talanoaga
O le pathophysiological process o le VAD e manatu e amata i le faʻaleagaina o sela i le medial-adventitial border o le vertebral artery, e mafua ai le atinaʻeina o le microhaematomata i totonu o le puipui o le alatoto ma, mulimuli ane, o loimata. Lenei mafai ona taitaiina atu i leakage o le toto i le arterial pa, mafua ai le vaʻaia o le lumen ma mulimuli ane thrombus fausiaina ma embolisation, mafua ai i le faʻamaʻi fesoʻotaʻi ma se tasi o lala o le vertebral alatoto. O lenei gaioiga faʻasolosolo e tutusa ma le vaʻaia o le carotid artery dissection, spontaneous thoracic aortic dissection ma spontaneous coronary artery dissection. O nei tuutuuga uma e foliga mai e tupu i talavou matutua ma o nisi ua taumatemate e ono avea i latou ma vaega o le masani ai faʻasologa pathophysiological gaioiga. Mataʻina i lenei tulaga o le mea moni o le tagata matua onosai onosaʻi a faʻasolosolo tuʻumamaina sela (atonu o se dissection) i le tusa o le tutusa tausaga (30? Tausaga) e pei o lenei onosaʻi ina ua ia iloa lona VAD.
E ui lava ina faʻafuaseʻi le faʻaleagaina, o le faʻavavega o le lumanaʻi ma faʻafitauli o le VAD e mafai ona faʻaauau le alualu i luma e taʻitaʻia ai le fesuiaʻiga o faʻamaoniga ma le faʻavae, e fuafua i le tulaga o le maʻi. O le faʻasesega lava ia, lea e atiina ae se taimi ao lei amataina le siama o le neural, e mafai ona mafua ai le faaosofia o ni faʻalogo mai le tino i totonu o le aluga, ma maua ai le tiga lea e sili ona lagona i le pito i luga o le totini poʻo le ulu. E naʻo le maeʻa ona faʻagasolo le faagasologa o le pathophiological agai i le tulaga o le faʻatonuina o le faʻaogaina poʻo le faʻasolosolo o le thrombus ma le faʻamalosia o le faʻalavelave, o le faʻaalia atoa o le faʻaleagaina. Ae ui i lea, e pei ona faʻaalia i lenei tulaga, o aʻafiaga o le neurological e mafai ona vave amataina i le faagasologa, aemaise lava i mataupu ia o lo o faaalia ai le lumanaʻi moni o le faʻaitiitia o le faʻaitiitia o le maualuga o le lua i le faʻamalosi.
There are several interesting aspects to this case. First, it highlights the importance of spine clinicians being alert to the possibility that what may appear to be typical �mechanical� neck pain could be something potentially more sinister, such as VAD. The sudden onset of severe suboccipital pain, with or without headache, and accompanying brainstem related neurological symptoms, should alert the clinician to the possibility of VAD. As in the case reported here, patients with a history of migraine will typically describe the headache as different from their usual migraine. A careful neurological examination should be performed, looking for possible subtle neurological deficits, although the neurological examination will often be negative in the early stages of VAD.
Lona lua, o se tolu o faʻamaoniga na faʻalauteleina le atugaluga e ono ono oʻo i luma le tagata maʻi ile VAD. O le faʻailoga tolu e aofia ai: (1) faʻapitoa i le amataga o le tiga ogaoga o le tino; (2) ogaoga o le ulu tiga lea na ese le eseesega mai le ulu o le ulu o le migraine masani; ma (3) faʻataʻotoga o le neurological e aʻafia ai le brainstem (i le foliga o le faʻalavelave faʻafuaseʻi). E le gata i lea, o suʻesuʻega faʻaletagata faʻapitoa na le lelei. Ae ui i lea, o le talafaasolo- pito na lava le popole e vave vave ona suʻeina.
When VAD is suspected but no frank signs of stroke are present, immediate vascular imaging is indicated. While the optimal imaging evaluation of VAD remains controversial, MRA or CTA are the diagnostic studies of choice given their excellent anatomic delineation and ability to evaluate for complications (including infarction and changes in brain perfusion). Some advocate the use of Doppler ultrasound; however, it has limited utility given the course of the vertebral artery in the neck and limited evaluation of the vertebral arteries cephalad to the origin. Additionally, ultrasound imaging is unlikely to allow visualisation of the dissection itself and thus can be negative in the absence of significant arterial occlusion.
Third, this case is interesting in light of the controversy about cervical manipulation as a potential �cause� of VAD. While case reports have presented patients who have experienced stroke related to VAD after cervical manipulation, and case�control studies have found a statistical association between visits to chiropractors and stroke related to VAD, further investigation has indicated that the association is not causal. Cassidy et al found that a patient who experiences stroke related to VAD is just as likely to have visited a primary care practitioner as to have visited a chiropractor prior to having the stroke. The authors suggested that the most likely explanation for the statistical association between visits to chiropractors and subsequent VAD is that a patient who experiences the initial symptoms of VAD (neck pain with or without headache) seeks medical attention for these symptoms (from a chiropractor, primary care practitioner, or another type of practitioner), then subsequently experiences the stroke, independent of any action taken by the practitioner.
It is important to note that, while there have been reported cases of carotid artery dissection after cervical manipulation, case�control studies have not found this association. The initial symptoms of carotid dissection (neurological symptoms, with neck and head pain less common than VAD), aortic dissection (sudden onset of severe, �tearing� pain) and coronary artery dissection (acute severe chest pain, ventricular fibrillation) are likely to cause the individual to immediately seek ED care, rather than seek chiropractic care. However, VAD has seemingly benign initial symptoms�neck pain and headache�which are symptoms that commonly cause patients to seek out chiropractic care. This may explain why only VAD is associated with visits to chiropractors, while these other types of dissections are not; patients with these other conditions, which have much more alarming symptoms, simply do not present to chiropractors.
This case is a good example of a patient with VAD in progress presenting to a chiropractor for the purpose of seeking relief from neck pain. Fortunately, the chiropractor was astute enough to ascertain that the patient’s symptoms were not suggestive of a �mechanical� cervical spine disorder, and appropriate diagnostic investigation was performed. However, if manipulation had been performed, the VAD that was already in progress from natural history may have been blamed on manipulation, after being detected on MRA imaging. Fortunately, in this case, the chiropractor was able to assist with early detection and treatment, and subsequently a stroke was likely averted.
Manatu e Aoao ai
- O se mataupu na tuʻuina atu lea na vaʻai ai se tagata maʻi i se tagata vaʻaia, aʻo sailia togafitiga mo le tiga o le ua, ma na fafaguina ai le popolega mo le faʻamalosia o le faʻavae o le uaea (VAD).
- Nai lo le faia o togafitiga togafitiga, na faasino atu e le fomaʻi le tagata gasegase mo ata maualuluga, lea na faʻamaonia ai le faʻamaoniga o le VAD.
- O le faʻataʻitaʻiga o loʻo faʻaalia ai le taua o le gauai atu i mea iloga talafaasolopito o tagata mamai ma le VAD.
- E avea foi ma se faʻataʻitaʻiga o se tagata gasegase i le VAD o loʻo faʻaauau pea ona sailia le auʻaunaga a se tagata vaʻaia mo uluai faailoga o le maʻi.
- I lenei tulaga, na amata vave ona iloa le faalavelave ma o le tagata gasegase sa toe malosi atoatoa e aunoa ma se isi itu.
tautinoga
O tusitala e fia faʻamaonia le fesoasoani a Pierre Cote, DC, PhD, mo lana fesoasoani ma le toe iloiloina o lenei tusitusiga.
Faamatalaga Faʻamatalaga
sao: O le au tusitala uma latou te faailoa mai ua latou saofagā i le tusiga o lenei tusitusiga: o le mafaufau ma le mamanu, o le tusiaina o tusitusiga, o toe iloiloga taua o tusitusiga, tusitusiga ma iloiloga, ma le faitau faʻamaonia o le tusitusiga mulimuli.
Tauvaga malie: Leai se tasi na faʻaalia.
Maliega o le tagata maʻi: Maua.
Faʻaaliga ma iloiloga a tupulaga: Faʻamaonia; fafo atu o tupulaga.
Faʻamatalaga mai le National Center for Biotechnology Information (NCBI). O le lautele o a tatou faʻamatalaga e faʻapulaʻaina i le faʻamaʻi faʻamaʻi faʻapea foi ma manua ma tuʻutuʻu. Ina ia talanoaina le mataupu, faamolemole ia lagona le saoloto e fesili ia Dr. Jimenez pe faʻafesoʻotaʻi mai i matou 915-850-0900 .
Cited by Dr. Alex Jimenez

Avanoa Faaopoopo: Lelei
O le soifua maloloina atoa ma le soifua maloloina e taua i le tausia o le paleni lelei faalemafaufau ma le faaletino i le tino. Mai le 'aiina o mea paleni paleni ma le faʻamalositino ma le auai i gaoioiga faaletino, o le moe i se taimi ola maloloina o le taimi ile masani ai, mulimuli i le soifua maloloina sili atu ma le soifua maloloina lelei e mafai ona fesoasoani i le tausia o le soifua manuia lautele. O le 'ai tele o fualaau aina ma fualaʻau e mafai ona uia se auala umi e fesoasoani ai i tagata ia ola maloloina.

TULAGA FAATINO: TUʻUʻUGA FAʻATASI: Tausia Sciatica Pain